idiopathic pulmonary fibrosis
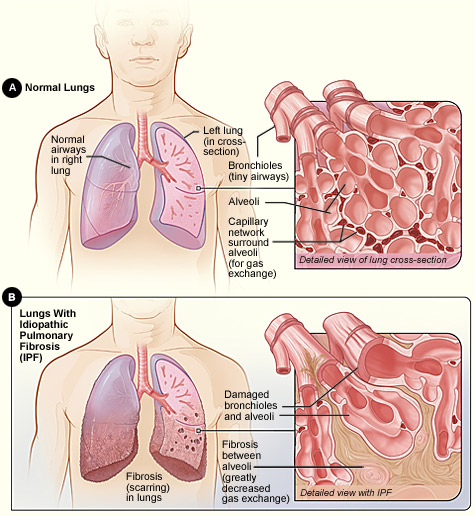
Figure A shows the location of the lungs and airways in the body. The inset image shows a detailed view of the lung's airways and air sacs in cross-section. Figure B shows idiopathic pulmonary fibrosis (scarring) in the lungs. The inset image shows a detailed view of the fibrosis and how it damages the airways and air sacs.
Pulmonary fibrosis is a condition in which tissue deep in the lungs becomes thick and stiff, or scarred, over time. The development of the scarred tissue is called fibrosis.
As the lung tissue becomes thicker, the lungs lose their ability to move oxygen into the bloodstream, and the brain and other organs don't receive the oxygen they need.
In some cases, doctors can find out what is causing the fibrosis. But in most cases, they can't find a cause. They call these cases idiopathic pulmonary fibrosis (IPF).
IPF is a serious condition. About 200,000 Americans have it. About 50,000 new cases are diagnosed each year. IPF affects mostly people 50 to 75 years of age.
IPF varies from person to person. In some people, the lung tissue quickly becomes thick and stiff. In others, the process is much slower, and in some people, the condition stays the same for years.
There is no cure for IPF yet. Many people live only about 3 to 5 years after diagnosis. The most common cause of death related to IPF is respiratory failure. Other causes include:
Some people may be more likely to develop IPF because of their genes (the basic units of heredity). If more than one member of your family has IPF, the condition is called familial idiopathic pulmonary fibrosis.
Today, scientists are beginning to understand more about what causes IPF, and they can diagnose it more quickly. They also are studying several medicines that may slow the progress of the disease. These efforts should lead to longer and better quality lives for people with IPF.
Causes
Doctors don't know what causes idiopathic pulmonary fibrosis (IPF). They think that something inside or outside of the lungs attacks the lungs again and again over time. These attacks injure the lungs and cause scarring in the tissue inside and between the air sacs. This makes it harder for oxygen to pass through the alveoli (air sac walls) into the bloodstream.
Doctors think the following things may increase your chances of developing IPF:
· Medicines to keep your heartbeat regular (for example, amiodarone or propranolol)
· Chemotherapy or cancer medicines, such as methotrexate, cyclophosphamide, and bleomycin
Your genes may also play a role in the development of IPF. Some families have at least two members with IPF.
Scientists have found that 9 out of 10 people with IPF also have gastroesophageal reflux disease (GERD). As a result, some scientists think that some people who have GERD may breathe in tiny drops of acid from their stomachs on a regular basis. The acid may then injure the lungs and lead to IPF. More research must be done to confirm this.
Signs and symptoms
The signs and symptoms of idiopathic pulmonary fibrosis (IPF) develop over time. They may not even begin to appear until the disease has done serious damage to your lungs. Once they do appear, they are likely to become worse over time.
The most common signs and symptoms are:
Other signs and symptoms that you may develop over time include:
IPF may lead to other medical conditions, including: collapsed lung, lung infections, blood clots in the lungs, and lung cancer.
As your condition gets worse, you may develop other potentially life-threatening conditions, including respiratory failure, pulmonary arterial hypertension, and heart failure.
Diagnosis
Idiopathic pulmonary fibrosis (IPF) produces the same kind of scarring and symptoms as some other lung diseases. This makes it hard to diagnose. Seeking medical help, preferably from a pulmonologist (a doctor who specializes in lung problems), as soon as you have symptoms is important.
To diagnose IPF, your doctor will ask about your medical history, perform a physical exam, and do several tests to rule out other causes of your symptoms and learn how badly your lungs are damaged.
Medical history
A complete medical history is important. Your doctor will ask about:
Diagnostic tests
There is no single test for diagnosing IPF. Your doctor will probably conduct several different tests, including the following.
A chest X-ray takes a picture of your heart and lungs. It can show shadows that suggest scar tissue. Many people with IPF have normal chest X-rays at the time they're diagnosed.
High-resolution
computerized tomography
High-resolution computerized tomography (HRCT) scan is an X-ray that provides sharper and more detailed images than a regular chest X-ray. It can show scar tissue and how much lung damage you have. This test can help your doctor spot IPF at an early stage or rule it out. It also can help your doctor decide how likely you are to respond to treatment.
Your doctor will do a lung function test called spirometry to find out how much lung damage you have. A spirometer is a device that measures how much air you can blow out of your lungs after taking a deep breath. It also measures how fast you can breathe the air out. If there is a lot of scarring in your lungs, you will not be able to move a normal amount of air out of them.
In pulse oximetry, your doctor attaches a small device to your finger or earlobe to see how much oxygen is in your bloodstream.
The doctor takes a small amount of blood from an artery in your arm, usually in your wrist. It's then checked for oxygen and carbon dioxide levels. This test is a more accurate way to check the level of oxygen in your bloodstream. Your blood can also be tested to see whether you have an infection that may be causing your symptoms.
Skin test for tuberculosis
Your doctor injects a small amount of a substance that reacts to tuberculosis (TB) under the top layer of skin on one of your arms. If you have a positive reaction, a small hard lump will develop at the injection site 48 to 72 hours after the test. This test is done to rule out TB.
Exercise
testing
Exercise testing is used to find out how well your lungs move oxygen and carbon dioxide in and out of your bloodstream when you're active. During this test, you walk or pedal on an exercise machine for a few minutes. Electrodes attached to your chest and an EKG (electrocardiogram) machine show your heart rate, a blood pressure cuff monitors your blood pressure, and a pulse oximeter attached to a finger or ear lobe shows how much oxygen is in your blood.
Sometimes doctors place a catheter in an artery in one of your arms to draw samples of your blood that will provide a more accurate measure of the oxygen and carbon dioxide in it. They may also ask you to breathe into a tube that separates the air you breathe out from room air and provides a precise measure of the amount of oxygen you've taken in and carbon dioxide you're breathing out.
Lung biopsy
Looking at samples of tissue from several places in your lungs under a microscope is the best way for your doctor to diagnose IPF. A lung biopsy can help your doctor rule out other causes of your condition, such as sarcoidosis, cancer, or infection. It can also show your doctor how far your condition has advanced. Doctors use several different procedures to obtain samples of your lung tissue:
Treatment
The goals of treating idiopathic pulmonary fibrosis (IPF) are to prevent more lung scarring, relieve your symptoms, maintain your ability to be active and get around, keep you healthy, and improve your quality of life.
Treatment can't remove scarring that has already happened. As a result, diagnosing and treating IPF as early as possible, before a lot of scarring has taken place, is very important.
Treatment is usually based on your age, medical history, any medical problems you may have, and how much the IPF has advanced.
Treatments can include:
Medicines
The main treatment for IPF is medicine to reduce inflammation. Many doctors also add a medicine to suppress your body's immune system. These treatments can prevent further scarring and increase survival time in some people, but they don't work for everyone.
Prednisone
The anti-inflammatory medicine that most doctors prescribe is high-dose prednisone, a corticosteroid. You usually take prednisone by mouth every day. Sometimes your doctor may give it to you through a needle or tube inserted into a vein in your arm for several days. After that, you usually take it by mouth.
Because prednisone can cause serious side effects, your doctor may prescribe it for only 3 to 6 months at first. Then, if it works for you, your doctor may reduce the dose over time and keep you on it for a longer time.
Most people who take high-dose prednisone for a long time can have side effects, including difficulty sleeping at night (insomnia), weight gain, acne, and irritability. Using prednisone for a long time also can lead to other conditions, including:
Prednisone also can cause conditions such as diabetes and glaucoma to get worse.
Other medicines
Many doctors prescribe a second medicine with prednisone.
· Nausea, vomiting, diarrhea, and fever and chills
· Anemia and low platelet and white blood cell counts
· Liver problems
· Pancreatitis or lymphoma (rarely)
The most common side effect of cyclophosphamide is a decrease in the number of blood cells that you have. This increases your chances for infection. Your doctor may order blood tests before, during, and after your treatment to see how your blood cells are affected by the drug. Other side effects can include: · Infertility in both men and women.
· Nausea, diarrhea, and fatigue (tiredness).
· Hair loss.
· Bladder irritation. Some people who have taken cyclophosphamide for more than 2 years have developed bladder cancer. If you take cyclophosphamide, you should drink at least 8 glasses of water a day. Your doctor should test your urine at least monthly.
Other medicines that may help people with IPF include the following:
New medicines being studied
Researchers are studying new treatments for IPF. Some are looking at medicines that may reduce inflammation and/or prevent or reduce scarring in IPF. These include medicines that are used to treat other conditions.
N-acetylcysteine. N-acetylcysteine is an antioxidant that's used mostly to thin mucus in patients with other lung conditions. A recent study showed that adding it to prednisone and azathioprine helped prevent further damage to the lungs of people with IPF.
Interferon gamma-1b. Interferon gamma-1b is a man-made version of a substance that your body normally produces to help fight infections. The drug is usually injected under your skin three times a week. The most common side effects include fever, headache, muscle soreness, fatigue, and chills.
Etanercept. Etanercept is a medicine that's used to reduce signs and symptoms of active arthritis or rheumatoid arthritis, such as joint swelling, pain, tiredness, and morning stiffness. Etanercept is also used to slow the progress of arthritis. The most common side effects are chills, cough, fever, sneezing, and sore throat.
Bosentan. Bosentan is a medicine developed to reduce high blood pressure in the blood vessels of the lungs (pulmonary arterial hypertension). You usually take this drug by mouth once or twice a day. The most common side effects include headaches, flushing, leg swelling, dizziness and fatigue, and liver problems. If you take this medicine, your doctor should test your blood often to monitor how your liver is working.
Imatinib. Imatinib is a medicine developed to treat a type of leukemia. The drug is usually given by mouth once a day. The most common side effects include fluid retention (swelling), nausea, vomiting, diarrhea, muscle cramping, and liver problems. If you take this medicine, your doctor should do frequent blood tests.
Sildenafil. Sildenafil is a medicine that is used to treat pulmonary arterial hypertension and erectile dysfunction. It usually has few side effects.
Pirfenidone. Pirfenidone is a medicine that may decrease scarring. The drug is usually taken by mouth three times a day. The most common side effects include a rash and sun sensitivity, nausea, vomiting, loss of appetite, drowsiness, and fatigue.
Colchicine. Colchicine is a medicine that has been used to prevent or treat attacks of gout. It may slow scarring in IPF. You usually take it by mouth once or twice a day. The side effects are generally less serious than those from prednisone. They may include nausea, vomiting, stomach pain, and diarrhea.
Methotrexate. Methotrexate is an immune system suppressant that's used to treat some cancers and autoimmune diseases. Most people take it once a week by mouth or injection. People with IPF usually take it for at least 4 to 6 months to see if it works. You may have side effects, especially if you take it at high doses.
The most serious possible side effect is liver damage. Your doctor should monitor how your liver is working every month that you're on this drug. If you take methotrexate for more than 2 years, you may want to have a liver biopsy to make sure your liver hasn't been damaged and that you can continue to take the medicine.
Other side effects may include nausea, mouth sores, skin rash, a decrease in infection-fighting white blood cells (requiring regular blood tests to check white cell levels), and an allergic reaction in the lungs that goes away when you stop taking the drug (this is very rare).
Your doctor should also monitor your white blood cells each month while you're on methotrexate. You can often reduce your chances of having bad side effects from methotrexate by taking folic acid.
Penicillamine. Penicillamine is used to treat rheumatoid arthritis and to prevent kidney stones. It's available in pill or capsule form. Several small studies have shown that penicillamine can improve lung function in some IPF patients, but more research is needed.
Penicillamine can cause serious side effects. The most common include nausea, vomiting, diarrhea, dyspepsia, and anorexia.
Cyclosporine. Cyclosporine is another immune system suppressant. It's used mostly to prevent rejection of kidney, liver, and heart transplants. Some doctors think it may help people with IPF reduce their dose of corticosteroids while waiting for a lung transplant. More research is needed.
Oxygen therapy
When the amount of oxygen in your blood gets low, you may need oxygen therapy to help reduce your shortness of breath and let you be more active. Oxygen is usually given through nasal prongs or a mask. At first, you may need it only during exercise and sleep. As your condition gets worse, you may need it all the time.
Pulmonary rehabilitation
Pulmonary rehabilitation is now the standard of care for people with ongoing lung disease. It usually involves treatment by a team of specialists in a specialized clinic. The goal is to teach you how to manage your condition and function at your best.
Services usually include:
Lung transplantation
Early referral for surgery to replace one of your lungs with a healthy lung from a human donor is usually recommended if you:
Single lung transplantation can improve your quality of life and help you live longer.
Complications can include rejection by the body of the transplanted lung and infection. You may have to take medicines for life to reduce the chances that your body will reject the transplanted lung.
Because the supply of donor lungs is limited, asking for an evaluation for a transplant as soon as possible is important.
Living with idiopathic pulmonary fibrosis
There is no cure for idiopathic pulmonary fibrosis (IPF) yet. Understanding that your symptoms may get worse over time is important. As your symptoms get worse, you may not be able to do many of the things that you did before you had IPF.
If you're still smoking, the most important thing you can do is stop. Ask your doctor or nurse about smoking cessation programs and products that can help. Avoid secondhand smoke as well. Ask family members and friends not to smoke in front of you or in your home, car, or workplace.
Ongoing medical care is important. Treatment by a pulmonologist who specializes in IPF is usually recommended. These specialists are usually located at major medical centers.
Treatment may relieve your symptoms and even slow or stop the fibrosis (scarring). Following your treatment plan is very important. You should:
Being as active as you can is important to both your physical and mental health. It can help you maintain your strength and lung function and reduce stress. Try moderate exercise, such as walking or riding a stationary bike. Ask your doctor about using oxygen while you do this.
As your condition advances, use a wheelchair or motorized scooter, or stay busy with activities that aren't physical in nature.
As your condition worsens, you may need oxygen full time. Some people with IPF carry portable oxygen when they go out.
You should also follow a healthy diet. Eating smaller, more frequent meals may relieve stomach fullness, which can make it difficult to breathe. If you need help with your diet, ask your doctor to arrange for a dietitian to work with you.
Getting plenty of rest can increase your energy and help you deal with the stress of living with a serious disease like IPF.
Maintain a positive attitude. Practicing relaxation techniques may help you do this. It may also help you avoid excessive oxygen intake caused by tension or overworked muscles.
Join a support group to help you adjust to living with IPF. Talk to others who have the same symptoms so you can see how they're coping. To find a local support group, check your telephone directory or contact the Coalition for Pulmonary Fibrosis or the Pulmonary Fibrosis Foundation.
Avoid situations that can make your symptoms worse, such as traveling by air or living at or traveling to high altitudes where the air is thin and the amount of oxygen in the air is low.


