lung transplant
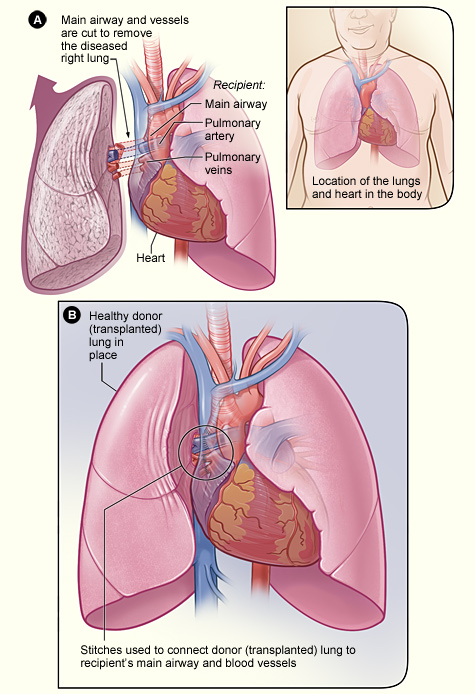
The process of a lung transplant. In figure A, the airway and blood vessels between a recipient's diseased right lung and heart are cut. In figure B, a healthy donor lung is stitched to the recipient's blood vessels and airway.
A lung transplant is surgery to remove a person's diseased lung and replace it with a healthy lung from a deceased donor. Lung transplants are done on people who are likely to die from lung disease within 1 to 2 years. Their conditions are so severe that other treatments, such as medicines or breathing devices, no longer work.
Overview
Lung transplants aren't very common due to the small number of donor organs available. Slightly more than 1,400 lung transplants were done in 2007. More donor lungs would mean a larger number of suitable lungs available for transplant.
Lung transplants most often are done in people aged 18 to 65. Sometimes this surgery is done in children and older adults. This article focuses on lung transplants in adults.
Each patient must go through a careful screening process to make sure he or she is a good candidate for a lung transplant. Donor lungs also are carefully screened to make sure they're healthy enough to be used in a transplant.
In the United States, the Organ Procurement and Transplantation Network (OPTN) manages the nationwide organ-sharing process. OPTN also maintains the waiting lists for all organ donations.
The number of people on the lung transplant waiting list constantly changes. About half of the people on the list receive a lung in any given year.
Some people get one lung during a transplant. This is called a single-lung transplant. Other people get two lungs. This is called a double-lung transplant.
Some people who have severe heart disease and lung disease get a heart and lung(s). This is called a heart-lung transplant.
A rare kind of lung transplant is a living donor lobar lung transplant. In this operation, a healthy adult donates a segment, or lobe, of one lung to another person. This type of transplant usually is done in children.
Outlook
Lung transplants are a "last resort" treatment for people who have severe disease and no other medical options. A lung transplant can improve a person's quality of life. For people who have certain lung problems, a transplant also may help them live longer than they would without the surgery.
Lung transplants have serious risks. Your body may reject the new lung, or you may develop infections. The short- and long-term complications of a lung transplant can be life threatening.
Who needs a lung transplant?
Your doctor may recommend a lung transplant if you have severe lung disease that's getting worse. If your condition is so serious that other treatments don't work, lung transplant may be the only option.
Lung transplants most often are used to treat people who have severe:
Applying to a lung transplant program
Lung transplants are done in medical centers (large hospitals) where the staff has a lot of organ transplant experience. In the US, if you need a lung transplant, you must apply to a center's transplant program.
Transplant teams at the medical center manage all aspects of the center's transplant program. Transplant team members may include a:
Other team members may include a social worker, psychiatrist, financial coordinator, and other specialists and medical personnel, such as a nutritionist and nurses.
The transplant team will need to find out whether you're a candidate for lung transplant. They will want to make sure you're healthy enough to have the surgery and go through a recovery program afterward.
To do this, they will ask about your medical history. The team will want to know whether you have other serious illnesses or conditions, such as cancer, HIV, or hepatitis. They also will ask whether you've had a major chest surgery before. A previous chest surgery may make it hard to do a lung transplant.
The team also will want to know whether you smoke or use alcohol or drugs.
You also will have tests to determine whether you're healthy enough for a lung transplant. Tests may include:
You'll talk with team members to make sure you're mentally and emotionally willing to accept the risks of the transplant process and later treatment. The team may ask whether you have a good support network of family and friends.
Before a lung transplant
In the United States, if you're accepted into a medical center's transplant program, you'll be placed on the Organ Procurement and Transplantation Network's (OPTN's) national waiting list. Your transplant team will work with you to make sure you're ready for the transplant if a donor lung becomes available.
Waiting for a donor lung can be frustrating. However, you can do several things to prepare.
While you wait for a lung, you may feel worried, scared, anxious, or depressed. These feelings are normal in this situation. Talk to your health care team about how you feel. They can offer suggestions for coping with your emotions. Family and friends also can offer support.
When a donor lung becomes available
OPTN matches a donor's lungs to a recipient based on need. OPTN will consider how severe a person's disease is and how quickly it's worsening. OPTN also will consider whether the transplant will improve the recipient's chances of survival, and by how much.
Organs are matched for blood type and the size of the donor lung and the recipient.
If OPTN and your transplant center think they have a good match for you, the center will call you and ask you to come in as soon as possible.
Once you arrive, your team will do tests to make sure you're healthy enough to have the surgery and that the lung is a good match. If you're healthy enough and the lung is a good match, the team will prepare you for surgery.
During a lung transplant
Just before the surgery, you will get general anesthesia. The term "anesthesia" refers to a loss of feeling and awareness. With general anesthesia, you will be asleep during the surgery and not feel any pain.
Once you're asleep, your doctors will make a small incision in your chest, and insert a central venous catheter into a vein. This tube allows easy access to your bloodstream. Doctors use it to deliver fluids and medicines to your body.
Your doctors also will insert a tube in your mouth and down your windpipe to help you breathe. They also will insert a tube in your nose and down to your stomach to drain contents from your stomach. A catheter will be used to keep your bladder empty.
The surgeon will make a cut in your chest to open it. He or she will then cut the main airway to your diseased lung and the blood vessels connecting your lung to your heart.
The surgeon will remove your diseased lung and place the donor organ in your chest. Then the surgeon will connect the main airway of the donor lung to your airway and its blood vessels to those of your heart.
If you're having a double-lung transplant, you may be connected to a heart-lung bypass machine. This machine takes over for your heart and pumps oxygen-rich blood to your body. During the surgery, the surgeon will remove your diseased lungs, one at a time, and replace them with the donor lungs.
A single-lung transplant usually takes 4 to 8 hours. A double-lung transplant usually takes 6 to 12 hours.
Some people may need a heart-lung transplant. A heart-lung transplant is surgery in which both the heart and lung(s) are replaced with healthy organs from a deceased donor. For this surgery, you're connected to a heart-lung bypass machine.
After a lung transplant
Recovery in the hospital
After surgery, you'll go to the hospital's intensive care unit (ICU) for at least several days. The tubes that were inserted before surgery will remain for a few days. The tube in your windpipe helps you breathe. Other tubes deliver medicines to, and drain fluids from, your body. You also will have sticky patches called electrodes attached to your chest to monitor your heart.
After leaving the ICU, you'll go to a hospital room. The staff will carefully watch your recovery.
You'll be taught how to do deep breathing exercises with a spirometer spirometry. This is a machine with a tube that you breathe into. When you breathe into the tube, the spirometer measures how much air your lungs can hold. It also measures how fast you can blow air out of your lungs after taking a deep breath.
You'll need to cough often. Coughing helps clear fluids from your lungs so they can work properly. A nurse will show you how to hold a pillow tightly near your incision area while you cough to help decrease discomfort.
Your immune system will regard your new lung as a foreign object and create antibodies (proteins) against the lung. This may cause your body to reject the new organ. To prevent this, your doctor will prescribe medicines to suppress your immune system. These medicines are called immunosuppressants.
Because these medicines weaken your immune system, you're more likely to get an infection after the transplant. Your medical team will take steps to prevent infection while you're in the hospital.
On average, people who have a lung transplant stay in the hospital from 1 to 3 weeks. However, some people have complications and stay much longer.
Recovery after leaving the hospital
Before you leave the hospital, your medical team will teach you how to keep track of your overall health. You'll learn how to watch your weight and take your blood pressure, pulse, and temperature.
Staff also will show you how to check your lung function. If you have diabetes, you'll learn how to test your blood sugar. You'll also learn the signs of the two main complications of lung transplant surgery: rejection and infection.
For the first 3 months after surgery, you'll go to the hospital often for blood tests, chest X-rays, lung function tests, and other tests. After 3 months, if you're doing well, you'll visit less often.
Making healthy lifestyle choices is very important. Not smoking, following a healthy diet, and following your doctor's advice on using alcohol will help you recover and stay as healthy as possible.
A healthy diet includes a variety of fruits, vegetables, and whole grains. It also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, trans fat, cholesterol, sodium (salt), and added sugar.
Your doctor may recommend an exercise program when you're able to do physical activity.
Emotional issues
Having a lung transplant may cause fear, anxiety, and stress. While you're waiting for a lung transplant, you may worry that you won't live long enough to get a new lung. After surgery, you may feel overwhelmed, depressed, or worried about complications.
All of these feelings are normal for someone going through major surgery. It's important to talk about how you feel with your health care team. Talking to a professional counselor also can help. If you're feeling very depressed, your health care team or counselor may prescribe medicines to make you feel better.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
Risks of lung transplant
A lung transplant can improve your quality of life and extend your lifespan. The first year after the transplant is the most critical. This is when the risk for complications is the highest.
In recent years, short-term survival from lung transplant has improved. Figures from 2005 on single-lung transplant show that:
Survival rates for double-lung transplants are similar. Talk with your doctor about what these figures may mean for you.
Complications
The major complications of lung transplant are rejection and infection.
Rejection
Your immune system will regard your new lung as a "foreign object." It will create antibodies (proteins) against the lung. This may cause your body to reject the new organ.
To prevent this, your doctor will prescribe medicines called immunosuppressants to suppress your immune system. You will need to take these medicines for the rest of your life.
Rejection is most common in the first 6 months after surgery, but it can happen any time after the transplant. Rejection can develop slowly or suddenly. Your doctor will teach you how to recognize possible signs and symptoms of rejection. If you know these signs and symptoms, you can seek treatment right away.
Signs and symptoms of rejection include:
If you have any of these signs or symptoms, seek medical care. Your doctor may prescribe medicines to treat the rejection and prevent complications.
These medicines may cause side effects, such as headaches, nausea (feeling sick to your stomach), and flu-like symptoms. If you have side effects, talk to your doctors. They may be able to change your medicine or adjust the doses.
Infection
The medicines you take to prevent the rejection of your new lung may weaken your immune system. As a result, you're more likely to get infections.
While you're in the hospital, staff will take special steps to prevent you from getting infections. After you leave the hospital, you also can take steps to prevent infection:
Other risks
Long-term use of immunosuppressants can cause diabetes, kidney damage, and osteoporosis (thinning of the bones). These medicines also can increase the risk of cancer. Talk to your doctor about the long-term risks of using immunosuppressants.


