THE HEALTH REVOLUTION: Surgery and Medicine in the Twenty-first Century - 5. Restoring Sight and Hearing

Figure 1. An eye operation being carried out with microsurgical techniques. A close-up of the patient's eye, as seen through the surgeon's microscope, appears on the monitor.
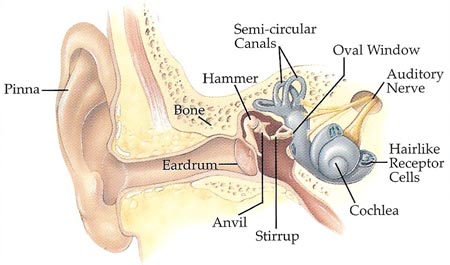
Figure 2. Inside the human ear.
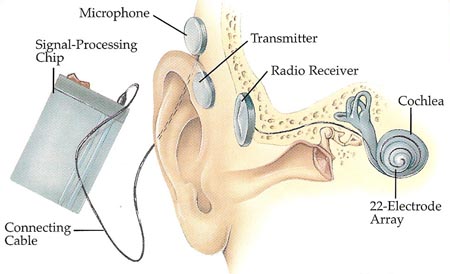
Figure 3. Cochlear implant.
Until recently, very little could be done to help people who were blind or profoundly deaf. But now medical science has developed a number of ways to restore partial hearing or sight to those who have lost or have never been able to use these senses.
One of the simplest of the new techniques is to replace a defective lens in the eye with a plastic substitute. For a variety of reasons, the natural lens in a person's eye may become cloudy. This cloudiness, known as a cataract, stops light from entering the eye and in severe cases results in almost total blindness. To correct the problem, with the aid of a microscope a surgeon opens up the clear part of the front of the eye – the cornea. The surgeon then removes the patient's diseased lens, which lies behind the cornea. Next, an artificial lens is put in the place of the natural one.
Sight Repairs
A number of other operations are now routinely carried out to repair damage to the eyes and restore normal vision (see Figure 1). At the back of the eye is a light-sensitive layer called the retina. The cells of the retina transmit vision signals to cells behind the retina. If the retina becomes torn or detached through an accident or disease, a person may become partly or completely blind. However, by using a narrow laser beam, a surgeon can effectively weld the damaged areas back into place.
Specialized lasers play an important part in the treatment of a serious eye condition known as glaucoma. In glaucoma, the pressure of the liquid inside the eyeball increases until it threatens to display a person's sight. By shining a laser through the cornea and burning a tiny hole in it, a surgeon can relieve the buildup of pressure without having to make a cut into the eye.
Damage to the cornea – the tough, clear outer covering of the center of the eye – can sometimes be repaired by a corneal transplant. This involves replacing the damaged section with a piece of healthy cornea taken from the eye of a donor. The operation calls for the finest sutures that are used in surgery, with suture thread no thicker than a human hair and needles less than a quarter of an inch long.
In 1995, surgeons in the United States began testing a bionic eye, which contains a miniature black and white TV camera. Signals are carried from the camera by a wire under the skin to a particular area of the skull. This area lies over the part of the brain that processes visual signals. The wire is attached to 256 tiny electrodes, each fitted to a small cluster of brain cells. In this way, it is hoped, electronic impulses from the camera will create visual images in the brain.
Hear, Hear
People who have limited hearing can have sounds made louder by a hearing aid. But just because the sounds are louder doesn't necessarily mean they are clearer. The problem is that ordinary hearing aids amplify all the sounds they pick up by the same amount. They don't allow for the fact that deafness affects different people in different ways.
Very often, people who are deaf can hear some frequencies of sound better than others. The frequency of sound determines pitch. For example, a high-frequency note has a high pitch. A low-frequency note has a low pitch. Deafness usually affects sounds of higher pitch more than sounds of lower pitch, which makes understanding speech, in particular, very difficult. To help get around this problem, researchers have developed hearing aids that can amplify some sounds more than others.
Important work in this field is being carried out at, among other places, the University of New Mexico in Albuquerque. The work is based o 30 years of investigation by scientists in the former Yugoslavia. These researchers studied the relationship between the understanding of speech and the frequencies of speech sounds. They also studied how different languages produce different sound frequencies. Based on their findings, the Yugoslav researchers developed a hearing aid that amplified sounds only at certain frequencies. Scientists at the University of New Mexico took this idea further by introducing computer technology so that the hearing aid could be reprogrammed to meet the needs of different users or the characteristics of different languages. The scientists called their invention the digital master hearing aid, or DMHA.
The first version of the DMHA, built in 1992, was about the size of a personal stereo, weighed just over 2 pounds, and was connected to a headset by a wire. The hearing aid worked with a special microchip that acted as a signal processor to boost the level of incoming sounds at selected frequencies. In the future the DMHA and devices like it will be developed further so they are smaller and lighter and are linked to the wearer's headset by radio signals instead of wires. A person requiring a hearing aid will visit a specialist and have his or her hearing tested across a wide range of frequencies. The information gathered from the test will be stored in a memory chip. Then the memory chip will be inserted into the hearing aid to customize it to the particular needs of the wearer. The memory chip will tell the signal-processing chip how much to boost the volume at each frequency to give the user a sense of hearing that is as near to normal as possible.
| Journey of a Sound Wave |
|---|
The fleshy outside part of the ear, called the pinna, collects sounds and helps us identify the sounds from which they come. The sound waves then travel down the auditory canal to the eardrum, a membrane that forms a barrier between the outer and the middle ear. When sound waves strike it, the eardrum vibrates, like the skin of a drum. Its vibrations are transmitted across the air-filled middle ear by the three smallest bones in the ear – the hammer, anvil, and stirrup. The stirrup is connected to a thin membrane, known as the oval window, which is set into the snail-shaped cochlea of the inner ear (see Figure 2). Vibrations of the oval window are detected by over 20,000 tiny hairs inside the cochlea. As these hairs vibrate, they stimulate nerve cells at their base. Signals from these nerve cells go up the auditory nerve to the brain, allowing us to hear. Joined to the cochlea are three semicircular canals, filled with fluid and set at right angles to one another, which help control our balance. |
Artificial Ears
The outer part of the ear is the simplest. When something goes wrong with the complicated parts that are hidden from view – the middle ear and the inner ear – then corrective action becomes difficult. In fact, until quite recently, to replace parts of the middle ear or inner ear would have been beyond the surgeon's power. Now, however, thousands of people every year are having their hearing at least partially restored, thanks to artificial implants.
As a result of a development in Japan, patients suffering from inflammation of the eardrum or middle ear can be given an artificial middle ear. Normally, sound passes down the channel of the outer ear to the eardrum. The eardrum vibrates, and the sound vibration is transmitted by three tiny bones in the middle ear to the cochlea.
The artificial middle ear developed in Japan bypasses the eardrum and the first two bones of the middle ear. Part of the device hooks behind the outside of the ear and converts sounds into magnetic signals that are picked up by a second component implanted within the skull. This second component transmits the signals along a wire to a vibrator placed in the middle-ear cavity. The vibrator then moves the third bone, known as the stirrup, which passes on this movement to the cochlea.
Cochlear Implants
Another new type of implant, called a cochlear implant, bypasses the eardrum and middle ear altogether and stimulates the cochlea directly (see Figure 3). It can help give people who are totally deaf some form of hearing, provided they have intact nerve fibers connecting the cochlea to the brain.
The cochlear implant consists of a tiny disk-shaped radio receiver with a long tail containing very fine wires. Dotted along the tail are a number of electrodes – little pieces of metal out of which an electric current can pass. A surgeon places the receiver beneath the skin, just behind the ear, and pushes the tail of the implant around the snail-like curl of the cochlea.
Outside the ear is a microphone that picks up sound. The signal is passed to a signal-processing chip that converts the sound into electrical impulses. These impulses are then sent to a tiny transmitter that sits behind the ear directly over the receiver. When the receiver picks up the processed sound signals, it passes them down to the electrodes inside the cochlea.
The earliest type of cochlear implant had only one electrode on the tail and was known as a single-channel implant. It stimulated the nerve fibers and sent just one electrical signal to the brain. The signal matched the sound waves picked up by the microphone, but it was left to the brain to try to sort out the frequency pattern, a job normally done by the cochlea.
More recent implants have a string of 22 or more electrodes along the tail, resting at different places in the cochlea. These mutlichannel devices depend on more sophisticated signal-processing chips that analyze the frequency pattern of sounds picked up by the microphone. Signals representing different sound frequencies are then sent to different parts of the cochlea, so the implant works in a manner closer to that of the natural ear.
Developments to Come
As miniature computers become ever more powerful, it will be possible to make replacement parts for ears and eyes that give a better and better quality of hearing and vision. Cochlear implants, for example, may eventually be able to analyze sounds in as much detail as a healthy human choc lea and so restore a person's hearing to normal. Similar advances in technology that allow visual scenes to be broken down into fine parts and turned into signals that can be fed along the optic nerve directly to the brain will allow blind people to see clearly.
Over the next few decades, it will become increasingly common for people to have defective or worn-out natural body parts replaced by artificial ones. This will allow accident victims, disabled people, and elderly people to live fuller, healthier, and longer lives.
But advances in surgery and medical care will also create a number of problems. The proportion of people of advanced age will steadily rise, which will place a strain of facilities and care for the elderly. The ability of people to pay for expensive implants may determine who is treated and who is not. And, finally, there is the ethical question of how much of a human being we are willing to replace by machinery. When it becomes possible, as it almost certainly will, to replace eyes, ears, even parts of the brain by electronic devices, will we want to place limits on what the surgeon should and should not do? If such limits are not imposed, will the time eventually come when, after repeated surgery, some people are more artificial than natural? And should that matter? These are questions that will need to be given serious consideration as we move through this century.

