breast cancer treatment

In breast-sparing surgery, the surgeon removes the tumor in the breast and some tissue around it. The surgeon may also remove lymph nodes under the arm. The surgeon sometimes removes some of the lining over the chest muscles below the tumor.
In total (simple) mastectomy, the surgeon removes the whole breast. Some lymph nodes under the arm may also be removed.
In modified radical mastectomy, the surgeon removes the whole breast, and most or all of the lymph nodes under the arm. Often, the lining over the chest muscles is removed. A small chest muscle also may be taken out to make it easier to remove the lymph nodes.
Many women with breast cancer want to take an active part in making decisions about their medical care. It is natural to want to learn all you can about your disease and treatment choices. Knowing more about breast cancer helps many women cope.
Shock and stress after the diagnosis can make it hard to think of everything you want to ask your doctor. It often helps to make a list of questions before an appointment. To help remember what the doctor says, you may take notes or ask whether you may use a tape recorder. You may also want to have a family member or friend with you when you talk to the doctor – to take part in the discussion, to take notes, or just to listen. You do not need to ask all your questions at once. You will have other chances to ask your doctor or nurse to explain things that are not clear and to ask for more details.
Your doctor may refer you to a specialist, or you may ask for a referral. Specialists who treat breast cancer include surgeons, medical oncologists, and radiation oncologists. You also may be referred to a plastic surgeon.
Treatment methods
Women with breast cancer have many treatment options. These include surgery, radiation therapy, chemotherapy, hormone therapy, and biological therapy. These options are described below. Many women receive more than one type of treatment.
The choice of treatment depends mainly on the stage of the disease. Treatment options by stage are described below.
Your doctor can describe your treatment choices and the expected results. You may want to know how treatment may change your normal activities. You may want to know how you will look during and after treatment. You and your doctor can work together to develop a treatment plan that reflects your medical needs and personal values.
Cancer treatment is either local therapy or systemic therapy:
Because cancer treatments often damage healthy cells and tissues, side effects are common. Side effects depend mainly on the type and extent of the treatment. Side effects may not be the same for each woman, and they may change from one treatment session to the next.
Before treatment starts, your health care team will explain possible side effects and suggest ways to help you manage them.
At any stage of disease, supportive care is available to control pain and other symptoms, to relieve the side effects of treatment, and to ease emotional concerns.
You may want to talk to your doctor about taking part in a clinical trial, a research study of new treatment methods. The section on "The promise of cancer research" has more information about clinical trials.
You may want to ask your doctor these questions before your treatment begins:
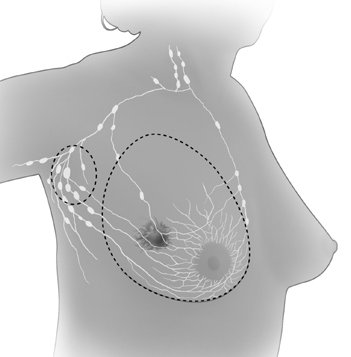
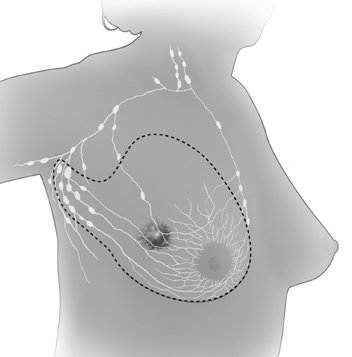
Surgery
Surgery is the most common treatment for breast cancer. There are several types of surgery. (See pictures below.) Your doctor can explain each type, discuss and compare the benefits and risks, and describe how each will change the way you look:
The surgeon often removes the underarm lymph nodes as well. A separate incision is made. This procedure is called an axillary lymph node dissection. It shows whether cancer cells have entered the lymphatic system.
After breast-sparing surgery, most women receive radiation therapy to the breast. This treatment destroys cancer cells that may remain in the breast.
Studies have found equal survival rates for breast-sparing surgery (with radiation therapy) and mastectomy for Stage I and Stage II breast cancer.
Sentinel lymph node biopsy is a new method of checking for cancer cells in the lymph nodes. A surgeon removes fewer lymph nodes, which causes fewer side effects. (If the doctor finds cancer cells in the axillary lymph nodes, an axillary lymph node dissection usually is done.) Information about ongoing studies of sentinel lymph node biopsy is in the section on "The promise of cancer research." These studies will learn the lasting effects of removing fewer lymph nodes.
You may choose to have breast reconstruction. This is plastic surgery to rebuild the shape of the breast. It may be done at the same time as a mastectomy or later. If you are considering reconstruction, you may wish to talk with a plastic surgeon before having a mastectomy. More information is in the "Breast reconstruction" section.
The time it takes to heal after surgery is different for each woman. Surgery causes pain and tenderness. Medicine can help control the pain. Before surgery, you should discuss the plan for pain relief with your doctor or nurse. After surgery, your doctor can adjust the plan if you need more relief. Any kind of surgery also carries a risk of infection, bleeding, or other problems. You should tell your health care provider right away if you develop any problems.
You may feel off balance if you've had one or both breasts removed. You may feel more off balance if you have large breasts. This imbalance can cause discomfort in your neck and back. Also, the skin where your breast was removed may feel tight. Your arm and shoulder muscles may feel stiff and weak. These problems usually go away. The doctor, nurse, or physical therapist can suggest exercises to help you regain movement and strength in your arm and shoulder. Exercise can also reduce stiffness and pain. You may be able to begin gentle exercises within days of surgery.
Because nerves may be injured or cut during surgery, you may have numbness and tingling in your chest, underarm, shoulder, and upper arm. These feelings usually go away within a few weeks or months. But for some women, numbness does not go away.
Removing the lymph nodes under the arm slows the flow of lymph fluid. The fluid may build up in your arm and hand and cause swelling. This swelling is lymphedema. Lymphedema can develop right after surgery or months to years later.
You will need to protect your arm and hand on the treated side for the rest of your life:
You should ask your doctor how to handle any cuts, insect bites, sunburn, or other injuries to your arm or hand. Also, you should contact the doctor if your arm or hand is injured, swells, or becomes red and warm.
If lymphedema occurs, the doctor may suggest raising your arm above your heart whenever you can. The doctor may show you hand and arm exercises. Some women with lymphedema wear an elastic sleeve to improve lymph circulation. Medication, manual lymph drainage (massage), or use of a machine that gently compresses the arm may also help. You may be referred to a physical therapist or another specialist.
You may want to ask your doctor these questions before having surgery:
Radiation therapy
Radiation therapy (also called radiotherapy) uses high-energy rays to kill cancer cells. Most women receive radiation therapy after breast-sparing surgery. Some women receive radiation therapy after a mastectomy. Treatment depends on the size of the tumor and other factors. The radiation destroys breast cancer cells that may remain in the area.
Some women have radiation therapy before surgery to destroy cancer cells and shrink the tumor. Doctors use this approach when the tumor is large or may be hard to remove. Some women also have chemotherapy or hormone therapy before surgery.
Doctors use two types of radiation therapy to treat breast cancer. Some women receive both types:
It is common for the skin in the treated area to become red, dry, tender, and itchy. Your breast may feel heavy and tight. These problems will go away over time. Toward the end of treatment, your skin may become moist and "weepy." Exposing this area to air as much as possible can help the skin heal.
Bras and some other types of clothing may rub your skin and cause soreness. You may want to wear loose-fitting cotton clothes during this time. Gentle skin care also is important. You should check with your doctor before using any deodorants, lotions, or creams on the treated area. These effects of radiation therapy on the skin will go away. The area gradually heals once treatment is over. However, there may be a lasting change in the color of your skin.
You are likely to become very tired during radiation therapy, especially in the later weeks of treatment. Resting is important, but doctors usually advise patients to try to stay as active as they can.
Although the side effects of radiation therapy can be distressing, your doctor can usually relieve them.
You may want to ask your doctor these questions before having radiation therapy:
Chemotherapy
Chemotherapy uses anticancer drugs to kill cancer cells. Chemotherapy for breast cancer is usually a combination of drugs. The drugs may be given as a pill or by injection into a vein (IV). Either way, the drugs enter the bloodstream and travel throughout the body.
Women with breast cancer can have chemotherapy in an outpatient part of the hospital, at the doctor's office, or at home. Some women need to stay in the hospital during treatment.
Side effects depend mainly on the specific drugs and the dose. The drugs affect cancer cells and other cells that divide rapidly:
Your doctor can suggest ways to control many of these side effects.
Some drugs used for breast cancer can cause tingling or numbness in the hands or feet. This problem usually goes away after treatment is over. Other problems may not go away. In some women, the drugs used for breast cancer may weaken the heart.
Some anticancer drugs can damage the ovaries. The ovaries may stop making hormones. You may have symptoms of menopause. The symptoms include hot flashes and vaginal dryness. Your menstrual periods may no longer be regular or may stop. Some women become infertile (unable to become pregnant). For women over the age of 35, infertility is likely to be permanent.
On the other hand, you may remain fertile during chemotherapy and be able to become pregnant. The effects of chemotherapy on an unborn child are not known. You should talk to your doctor about birth control before treatment begins.
Hormone therapy
Some breast tumors need hormones to grow. Hormone therapy keeps cancer cells from getting or using the natural hormones they need. These hormones are estrogen and progesterone. Lab tests can show if a breast tumor has hormone receptors. If you have this kind of tumor, you may have hormone therapy.
This treatment uses drugs or surgery:
The side effects of hormone therapy depend largely on the specific drug or type of treatment. Tamoxifen is the most common hormone treatment. In general, the side effects of tamoxifen are similar to some of the symptoms of menopause. The most common are hot flashes and vaginal discharge. Other side effects are irregular menstrual periods, headaches, fatigue, nausea, vomiting, vaginal dryness or itching, irritation of the skin around the vagina, and skin rash. Not all women who take tamoxifen have side effects.
It is possible to become pregnant when taking tamoxifen. Tamoxifen may harm the unborn baby. If you are still menstruating, you should discuss birth control methods with your doctor.
Serious side effects of tamoxifen are rare. However, it can cause blood clots in the veins. Blood clots form most often in the legs and in the lungs. Women have a slight increase in their risk of stroke.
Tamoxifen can cause cancer of the uterus. Your doctor should perform regular pelvic exams. You should tell your doctor about any unusual vaginal bleeding between exams.
When the ovaries are removed, menopause occurs at once. The side effects are often more severe than those caused by natural menopause. Your health care provider can suggest ways to cope with these side effects.
Biological therapy
Biological therapy helps the immune system fight cancer. The immune system is the body's natural defense against disease.
Some women with breast cancer that has spread receive a biological therapy called Herceptin® (trastuzumab). It is a monoclonal antibody. It is made in the laboratory and binds to cancer cells.
Herceptin is given to women whose lab tests show that a breast tumor has too much of a specific protein known as HER2. By blocking HER2, it can slow or stop the growth of the cancer cells.
Herceptin is given by vein. It may be given alone or with chemotherapy.
The first time a woman receives Herceptin, the most common side effects are fever and chills. Some women also have pain, weakness, nausea, vomiting, diarrhea, headaches, difficulty breathing, or rashes. Side effects usually become milder after the first treatment.
Herceptin also may cause heart damage. This may lead to heart failure. Herceptin can also affect the lungs. It can cause breathing problems that require a doctor at once. Before you receive Herceptin, your doctor will check for your heart and lungs. During treatment, your doctor will watch for signs of lung problems.
You may want to ask your doctor these questions before having chemotherapy, hormone therapy, or biological therapy:
Treatment choices by stage
Your treatment options depend on the stage of your disease and these factors:
Below are brief descriptions of common treatments for each stage. Other treatments may be appropriate for some women. Clinical trials can be an option at all stages of breast cancer. "The promise of cancer research" section has information about clinical trials.
Stage 0
Stage 0 breast cancer refers to lobular carcinoma in situ (LCIS) or ductal carcinoma in situ (DCIS):
Having LCIS in one breast increases the risk of cancer for both breasts. A very small number of women with LCIS try to prevent cancer with surgery to remove both breasts. This is a bilateral prophylactic mastectomy. The surgeon usually does not remove the underarm lymph nodes.
Stages I, II, IIIA, and operable IIIC
Women with Stage I, II, IIIA, and operable (can treat with surgery) IIIC breast cancer may have a combination of treatments. Some may have breast-sparing surgery followed by radiation therapy to the breast. This choice is common for women with Stage I or II breast cancer. Others decide to have a mastectomy.
With either approach, women (especially those with Stage II or IIIA breast cancer) often have lymph nodes under the arm removed. The doctor may suggest radiation therapy after mastectomy if cancer cells are found in 1 to 3 lymph nodes under the arm, or if the tumor in the breast is large. If cancer cells are found in more than 3 lymph nodes under the arm, the doctor usually will suggest radiation therapy after mastectomy.
The choice between breast-sparing surgery (followed by radiation therapy) and mastectomy depends on many factors:
Some women have chemotherapy before surgery. This is neoadjuvant therapy (treatment before the main treatment). Chemotherapy before surgery may shrink a large tumor so that breast-sparing surgery is possible. Women with large Stage II or IIIA breast tumors often choose this treatment.
After surgery, many women receive adjuvant therapy. Adjuvant therapy is treatment given after the main treatment to increase the chances of a cure. Radiation treatment can kill cancer cells in and near the breast. Women also may have systemic treatment such as chemotherapy, hormone therapy, or both. This treatment can destroy cancer cells that remain anywhere in the body. It can prevent the cancer from coming back in the breast or elsewhere.
Stages IIIB and inoperable IIIC
Women with Stage IIIB (including inflammatory breast cancer) or inoperable Stage IIIC breast cancer usually have chemotherapy. (Inoperable cancer means it cannot be treated with surgery.)
If the chemotherapy shrinks the tumor, the doctor then may suggest further treatment:
Stage IV
In most cases, women with Stage IV breast cancer have hormone therapy, chemotherapy, or both. Some also may have biological therapy. Radiation may be used to control tumors in certain parts of the body. These treatments are not likely to cure the disease, but they may help a woman live longer.
Many women have supportive care along with anticancer treatments. Anticancer treatments are given to slow the progress of the disease. Supportive care helps manage pain, other symptoms, or side effects (such as nausea). It does not aim to extend a woman's life. Supportive care can help a woman feel better physically and emotionally. Some women with advanced cancer decide to have only supportive care.
Recurrent breast cancer
Recurrent cancer is cancer that has come back after it could not be detected. Treatment for the recurrent disease depends mainly on the location and extent of the cancer. Another main factor is the type of treatment the woman had before.
If breast cancer comes back only in the breast after breast-sparing surgery, the woman may have a mastectomy. Chances are good that the disease will not come back again.
If breast cancer recurs in other parts of the body, treatment may involve chemotherapy, hormone therapy, or biological therapy. Radiation therapy may help control cancer that recurs in the chest muscles or in certain other areas of the body.
Treatment can seldom cure cancer that recurs outside the breast. Supportive care is often an important part of the treatment plan. Many patients have supportive care to ease their symptoms and anticancer treatments to slow the progress of the disease. Some receive only supportive care to improve their quality of life.
Breast reconstruction
Some women who plan to have a mastectomy decide to have breast reconstruction. Other women prefer to wear a breast form (prosthesis). Others decide to do nothing. All of these options have pros and cons. What is right for one woman may not be right for another. What is important is that nearly every woman treated for breast cancer has choices.
Breast reconstruction may be done at the same time as the mastectomy, or later on. If you are thinking about breast reconstruction, you should talk to a plastic surgeon before the mastectomy, even if you plan to have your reconstruction later on.
There are many ways to reconstruct the breast. Some women choose to have implants. Implants may be made of saline or silicone. The safety of silicone breast implants has been under review by the Food and Drug Administration (FDA) for several years. If you are thinking about having silicone implants, you may want to talk with your doctor about the FDA findings. Your doctor can tell you if silicone implants are an option.
You also may have breast reconstruction with tissue that the plastic surgeon moves from another part of your body. Skin, muscle, and fat can come from your lower abdomen, back, or buttocks. The surgeon uses this tissue to create a breast shape.
Which type of reconstruction is best depends on your age, body type, and the type of surgery you had. The plastic surgeon can explain the risks and benefits of each type of reconstruction.
You may want to ask your doctor these questions about breast reconstruction:
Complementary and alternative medicine
Some women with breast cancer use complementary and alternative medicine (CAM):
You may want to ask the doctor these questions before you decide to use CAM:
Acupuncture, massage therapy, herbal products, vitamins or special diets, visualization, meditation, and spiritual healing are types of CAM.
Many women say that CAM helps them feel better. However, some types of CAM may change the way standard treatment works. These changes could be harmful. And some types of CAM could be harmful even if used alone.
Nutrition and physical activity
It is important for women with breast cancer to take care of themselves. Taking care of yourself includes eating well and staying as active as you can.
You need the right amount of calories to maintain a good weight. You also need enough protein to keep up your strength. Eating well may help you feel better and have more energy.
Sometimes, especially during or soon after treatment, you may not feel like eating. You may be uncomfortable or tired. You may find that foods do not taste as good as they used to. In addition, the side effects of treatment (such as poor appetite, nausea, vomiting, or mouth sores) can make it hard to eat well. Your doctor, dietitian, or other health care provider can suggest ways to deal with these problems.
Many women find they feel better when they stay active. Walking, yoga, swimming, and other activities can keep you strong and increase your energy. Exercise may reduce nausea and pain and make treatment easier to handle. It also can help relieve stress. Whatever physical activity you choose, be sure to talk to your doctor before you start. Also, if your activity causes you pain or other problems, be sure to let your doctor or nurse know about it.
Follow-up care
Follow-up care after treatment for breast cancer is important. Recovery is different for each woman. Your recovery depends on your treatment, whether the disease has spread, and other factors.
Even when the cancer seems to have been completely removed or destroyed, the disease sometimes returns because undetected cancer cells remained somewhere in the body after treatment. Your doctor will monitor your recovery and check for recurrence of the cancer.
You should report any changes in the treated area or in your other breast to the doctor right away. Tell your doctor about any health problems, such as pain, loss of appetite or weight, changes in menstrual cycles, unusual vaginal bleeding, or blurred vision. Also talk to your doctor about headaches, dizziness, shortness of breath, coughing or hoarseness, backaches, or digestive problems that seem unusual or that don't go away. Such problems may arise months or years after treatment. They may suggest that the cancer has returned, but they can also be symptoms of other health problems. It is important to share your concerns with your doctor so problems can be diagnosed and treated as soon as possible.
Follow-up exams usually include the breasts, chest, neck, and underarm areas. Since you are at risk of getting cancer again, you should have mammograms of your preserved breast and your other breast. You probably will not need a mammogram of a reconstructed breast or if you had a mastectomy without reconstruction. Your doctor may order other imaging procedures or lab tests.
Sources of support
Learning you have breast cancer can change your life and the lives of those close to you. These changes can be hard to handle. It is normal for you, your family, and your friends to have many different and sometimes confusing feelings.
You may worry about caring for your family, keeping your job, or continuing daily activities. Concerns about treatments and managing side effects, hospital stays, and medical bills are also common. Doctors, nurses, and other members of the health care team can answer questions about treatment, working, or other activities. Meeting with a social worker, counselor, or member of the clergy can be helpful if you want to talk about your feelings or concerns. Often, a social worker can suggest resources for financial aid, transportation, home care, or emotional support.
Friends and relatives can be very supportive. Also, you may find it helps to discuss your concerns with others who have cancer. Women with breast cancer often get together in support groups to share what they have learned about coping with their disease and the effects of their treatment. It is important to keep in mind, however, that each woman is different. Ways that one woman deals with cancer may not be right for another. You may want to ask your health care provider about advice you receive from other women with breast cancer.
Several organizations offer special programs for women with breast cancer. Women who have had the disease serve as trained volunteers. They may talk with or visit women with breast cancer, provide information, and lend emotional support. They often share their experiences with breast cancer treatment, breast reconstruction, and recovery.
You may be afraid that changes to your body will affect not only how you look but also how other people feel about you. You may worry that breast cancer and its treatment will affect your sexual relationships. Many couples find it helps to talk about their concerns. Some find that counseling or a couples' support group can be helpful.
The promise of research
Doctors all over the country are conducting many types of clinical trials (research studies in which people volunteer to take part). They are studying new ways to prevent, detect, diagnose, and treat breast cancer. Some are also studying therapies that may improve the quality of life for women during or after cancer treatment.
Clinical trials are designed to answer important questions and to find out whether new approaches are safe and effective. Research already has led to advances and researchers continue to search for more effective methods for dealing with cancer.
Women who join clinical trials may be among the first to benefit if a new approach is effective. And even if people in a trial do not benefit directly, they still make an important contribution by helping doctors learn more about breast cancer and how to control it. Although clinical trials may pose some risks, researchers do all they can to protect their patients.
If you are interested in being part of a clinical trial, talk with your doctor. Trials are available for all stages of breast cancer.
Research on prevention
Scientists are looking for drugs that may prevent breast cancer. For example, they are testing several different drugs that lower hormone levels or prevent a hormone's effect on breast cells.
In one large study, the drug tamoxifen reduced the number of new cases of breast cancer among women who were at an increased risk of the disease. Doctors are studying whether the drug raloxifene is as effective as tamoxifen. This study is called STAR (Study of Tamoxifen and Raloxifene). Results will be available in late 2006.
Research on detection, diagnosis, and staging
At this time, mammograms are the most effective tool we have to detect changes in the breast that may be cancer. In women at high risk of breast cancer, researchers are studying the combination of mammograms and ultrasound. Researchers are also exploring positron emission tomography (PET) and other ways to make detailed pictures of breast tissue.
In addition, researchers are studying tumor markers. Tumor markers may be found in blood, in urine, or in fluid from the breast (nipple aspirate). High amounts of these substances may be a sign of cancer. Some markers may be used to check breast cancer patients for signs of disease after treatment. At this time, however, no tumor marker test is reliable enough to be used routinely to detect breast cancer.
Ductal lavage also is under study. This technique collects cells from breast ducts. A liquid flows through a catheter (very thin, flexible tube) into the opening of a milk duct on the nipple. The liquid and breast cells are withdrawn through the tube. A pathologist checks the cells for cancer or changes that may suggest an increased risk of cancer.
Research on treatment
Researchers are studying many types of treatment and their combinations:
In addition, researchers are looking at ways to lessen the side effects
from treatment, such as lymphedema from surgery. They are looking at ways
to reduce pain and improve quality of life. One method under study is sentinel
lymph node biopsy. Today, surgeons have to remove many lymph nodes under
the arm and check each of them for cancer. Researchers are studying whether
checking only the node to which cancer is most likely to spread (sentinel
lymph node) will allow them to predict whether cancer has spread to other
nodes. If this new procedure works as well as standard treatment, surgeons
may be able to remove fewer lymph nodes. This could reduce lymphedema for
many patients.


