melanoma

Melanoma.
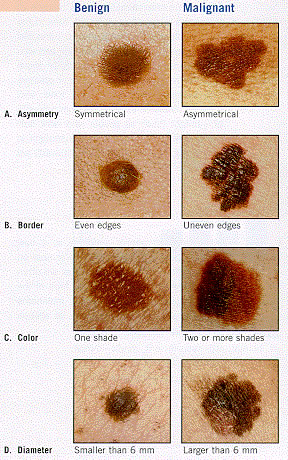
The ABCD rule for spotting a melanoma.
Melanoma is a form of skin cancer that begins in melanocytes – the cells that make the brown pigment melanin. Melanoma usually starts in a mole.
The skin is the body's largest organ. It protects against heat, sunlight, injury, and infection. The skin has two main layers: the epidermis (upper or outer layer) and the dermis (lower or inner layer).
Melanocytes are found throughout the lower part of the epidermis. They make melanin, the pigment that gives skin its natural color. When skin is exposed to the sun, melanocytes make more pigment, causing the skin to tan, or darken.
When melanoma starts in the skin, the disease is called cutaneous melanoma. Melanoma may also occur in the eye and is called intraocular or ocular melanoma.
Melanoma is the most aggressive of three types of skin cancer, the others being basal cell skin cancer and squamous cell skin cancer.
Where on the body does melanoma occur?
Melanoma can occur anywhere on the body.
In men, melanoma is often found on the trunk (the area from the shoulders
to the hips) or the head and neck. In women, melanoma often develops on
the arms and legs. Melanoma usually occurs in adults, but it is sometimes
found in children and adolescents.
What increases the risk of melanoma?
Unusual moles, exposure to sunlight, and health history can affect the risk of developing melanoma.
Anything that increases your risk of getting a disease is called a risk factor. Risk factors for melanoma include the following:
Signs and symptoms
Possible signs of melanoma include a change in the appearance of a mole or pigmented area.
These and other symptoms may be caused by melanoma or by other conditions. A doctor should be consulted if any of the following problems occur:
- changes in size, shape, or color
- has irregular edges or borders
- is more than 1 color
- is asymmetrical (if the mole is divided in half, the 2 halves are different in size or shape)
- itches
- oozes, bleeds, or is ulcerated (a hole forms in the skin when the top layer of cells breaks down and the underlying tissue shows through).
Here is the "ABCD rule" to help tell a normal mole from a melanoma:
Other important signs of melanoma include changes in size, shape, or color of a mole. Some melanomas do not fit the descriptions above, and it may be hard to tell if the mole is normal or not, so you should show your doctor anything that you are unsure of.
Diagnosis
Tests that examine the skin are used to detect (find) and diagnose melanoma.
If a mole or pigmented area of the skin changes or looks abnormal, the following tests and procedures can help detect and diagnose melanoma:
Suspicious areas should not be shaved off or cauterized (destroyed with a hot instrument, an electrical current, or a caustic substance).
What affects the chance of recovery?
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the following:
Although many people are successfully treated, melanoma can recur (come back). In recurrent melanoma, the cancer may come back at the original site or in other parts of the body, such as the lungs or liver.
Stages of melanoma
Stage 0
In stage 0, melanoma is found only in the epidermis (outer layer of the skin). Stage 0 is also called melanoma in situ.
Stage I
Stage I is divided into stages IA and IB.
- not more than 1 millimeter thick, with ulceration, and may have spread into the dermis or the tissues below the skin;
or
-1 to 2 millimeters thick, with no ulceration.
Stage II
Stage II is divided into stages IIA, IIB, and IIC.
- 1 to 2 millimeters thick, with ulceration; or
- 2 to 4 millimeters thick, with no ulceration.
- 2 to 4 millimeters thick, with ulceration; or
- more than 4 millimeters thick, with no ulceration.
Stage III
In stage III, the tumor may be any thickness, with or without ulceration, and:
Stage IV
In stage IV, the tumor may be any thickness, with or without ulceration, may have spread to 1 or more nearby lymph nodes, and has spread to other places in the body.
Tests done to diagnose the stage of melanoma
The process used to find out whether cancer has spread within the skin or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment.
The following tests and procedures may be used in the staging process:
The results of these tests are viewed together with the results of the tumor biopsy to determine the melanoma stage.


