bronchopulmonary dysplasia
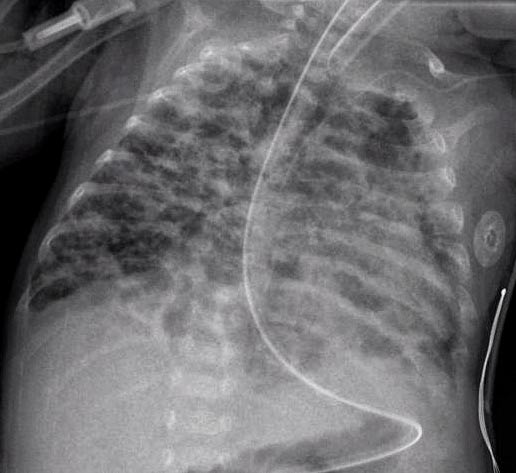
A chest radiograph of bronchopulmonary dysplasia.
Bronchopulmonary dysplasia (BPD) is a chronic lung disease of babies. BPD develops most commonly in the first 4 weeks after birth. BPD mostly occurs in babies who are born more than 4 weeks before their due dates, although sometimes the babies are full term. In BPD, the lungs do not work properly, and the babies have trouble breathing. They need extra oxygen and may even need help from a breathing machine. Doctors think babies develop BPD because their lungs are sensitive to something damaging in the environment, such as high levels of oxygen, a breathing machine, or an infection. Premature babies are also at risk for complications in other parts of the body that are not fully mature, including the heart, kidneys, brain, stomach, intestines, and eyes.
With new and better treatments today, most babies with BPD live. In severe cases, the baby may die.
BPD is different from respiratory distress syndrome (RDS), which occurs in the lungs of premature infants because their lungs do not produce enough surfactant (a liquid material that coats the inside of the lungs, making it easy to breathe). In the past, doctors thought that BPD was a disease mostly in babies who survived RDS. They believed that the treatment of RDS with a breathing machine and extra oxygen caused BPD. Today, babies with RDS are treated with surfactant replacement therapy and do very well. With this new treatment, BPD is not common in babies born early and weighing 3 pounds or more.
Causes
Bronchopulmonary dysplasia (BPD) does not develop in all infants for the same reasons. Doctors now believe that BPD occurs because of the way a particular baby's lungs respond to the outside environment in the first hours or days after birth. Whether BPD actually develops will depend on the immaturity of the lungs, the irritants in the environment, and other factors that may not be known, such as exposures in the womb or inherited traits. Factors that might contribute to BPD include:
The lungs in babies born earlier than 30 weeks are often not formed well enough to support breathing. The poorly formed lungs do not provide enough surface area or the fine network of blood vessels necessary to allow the oxygen from the air to travel into the blood stream, or for the carbon dioxide to travel from the blood across the surface of the lungs into the air. This process of oxygen and carbon dioxide transfer across the lungs is called gas exchange. Over time, the lungs may also develop other complications, which may make the gas exchange more difficult.
Many babies with breathing problems have low oxygen levels in the blood and are given extra oxygen to protect the brain, heart, liver, and kidneys from damage caused by low oxygen. However, high levels of extra oxygen can harm the lungs, cause inflammation, and slow or stop the lung growth in babies born very early. Babies who need a high level of extra oxygen for a period of time may develop BPD.
Babies who cannot breathe on their own have breathing failure. Many of these babies are put on a breathing machine to help them breathe. The machine pushes air into the baby's lungs. The pressure that the machine uses to push the air can irritate the airways and the lungs and cause them to become inflamed.
Babies can be exposed to infections both in the womb and after birth. Infections in babies born early can harm their less-formed lungs and cause them to become inflamed. Lung infections also increase the baby's need for extra oxygen and for help with breathing.
Risk for factors
Factors like lower weight and less time in the mother's womb can increase a baby's risk of developing bronchopulmonary dysplasia (BPD). Today, most babies with BPD (9 of 10) weigh 1,500 grams (about 3½ pounds), or less, at birth. Babies born weighing less than 1,000 grams (about 2 pounds) are at very high risk. About one of three of these babies develops BPD. These small babies can develop BPD even if they do not have respiratory distress syndrome or need a breathing machine.
Today, larger and more mature babies rarely develop BPD, due to better treatment of breathing problems in newborns. The larger and more mature babies who develop BPD usually have had serious and prolonged breathing problems in the first days of life.
About 5,000 to 10,000 babies in the United States develop BPD each year. Because more babies weighing less than 3 pounds live past 4 weeks, more babies develop BPD today than 30 years ago.
Signs and symptoms
Babies with bronchopulmonary dysplasia (BPD) struggle to breathe, and they show signs of distress that are found with other breathing problems. The severity of the signs of breathing difficulty will vary, depending on the severity of disease and lung maturity. These signs include:
If a baby develops any of the above signs of respiratory distress, the doctors will look for the cause, which might be BPD but also might be another respiratory problem. Doctors also have to make sure that the baby does not have a problem with the function of the heart.
Diagnosis
It is difficult to make a diagnosis of bronchopulmonary dysplasia (BPD) before a baby is about 14 to 30 days old. To diagnose BPD, doctors consider whether the baby had a lung injury within a few days of birth and continues to need extra oxygen after receiving oxygen treatment for a certain period of time. A chest X-ray may help confirm abnormal lung development.
Doctors will grade the severity of the BPD as mild, moderate, or severe depending on the amount and length of time the baby needs extra oxygen.
Treatment
No treatment is specific for bronchopulmonary dysplasia (BPD); rather, treatment is supportive. Doctors provide treatment to help the baby breathe better. They make sure the baby has enough oxygen; is properly fed, kept warm, and treated for infections; and is given the right amount of fluids and nourishment. This gives the baby's lungs time to mature. Babies with BPD are usually treated in a special intensive care unit (ICU) for newborns (neonatal ICU). Some babies may be treated in the neonatal ICU even before doctors know that the babies have BPD, because they may have been born premature, needed treatment for respiratory distress syndrome (RDS), or had other problems. Doctors can tell if a baby has BPD only after the baby is several weeks old.
Treatment for BPD is done in three stages. The stages are:
Treatments for babies who show signs of RDS but who are not yet diagnosed with BPD include:
Once doctors know a baby has BPD, some or all of the following treatments are continued in the ICU:
Today, most babies with BPD recover. They may spend several weeks or months in the hospital. However, the best place for a baby to grow and develop is at home with his or her family, in a loving and familiar environment. After the baby goes home:
Prevention
Small babies born very prematurely have the greatest chance of developing bronchopulmonary dysplasia. Programs of regular prenatal care for women at high risk of early delivery can lower the number of babies born early.
For some women, taking costeroid medications may lower the chance of having a premature or low-birth-weight baby. However, only one course of corticosteroid should usually be used for this purpose before birth.
Living with bronchopulmonary dysplasia
The signs and symptoms that continue after the baby leaves the hospital can vary. Babies with bronchopulmonary dysplasia (BPD) are more likely than other babies to get colds, flu, and other infections that generally are mild in most children but can be life-threatening in babies with BPD. They may also continue to need extra oxygen. Some may need to use a breathing machine throughout early childhood.
Babies who survive BPD are at higher risk for complications after the usual childhood infections. To be safe, they are often treated in the hospital for respiratory infections.
Babies who survive BPD may grow more slowly than normal. The slow growth often lasts into their second year of life. They usually remain smaller than normal children of the same age. Like most children, their lung growth is almost complete at 8 years of age. However, they may have some lasting problems with their lung function even when they are adults.
In very severe cases, they may have a small risk of some long-term problems. These include:
The risk of these problems is very small. Parents should not assume that their child will develop these problems. If they do occur, parents and families can get information about these problems from their doctors.
Parents can take a number of steps to help their babies recover and grow as normally as possible. These include:


