colonoscopy
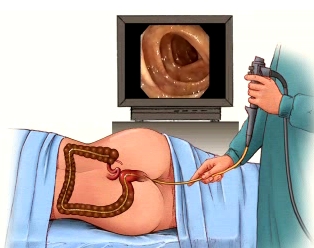
Colonoscopy is an internal examination of the colon (part of the large intestine) and rectum, using an instrument called a colonoscope. The colonoscope has a small camera attached to a flexible tube. Unlike sigmoidoscopy, which can only reach the lower third of the colon, colonoscopy examines the entire length of the colon.
The patient lies on his or her left side with knees drawn up toward the chest. A sedative and pain reliever is administered, and the colonoscope is inserted through the anus and gently advanced to the lowest part of the small bowel. Air is inserted through the scope to provide a better view. Suction may be used to remove fluid or stool.
Because the colonoscope provides a better view as it is withdrawn, a more careful examination is done while the scope is being pulled out. Tissue samples may be taken with tiny biopsy forceps inserted through the scope. Polyps may be removed with electrocautery snares, and photographs may be taken. Specialized procedures, such as laser therapy, may also be done.
Preparation for colonoscopy
It is essential that the bowel be completely cleansed before colonoscopy. The patient is given instructions for doing this. Preparation may include a combination of enemas, not eating solid foods for 2 or 3 days before the test, and taking laxatives. Patients will usually be told to avoid taking aspirin, ibuprofen, naproxen, or other blood-thinning medications for several days before the test. They will be asked to drink plenty of clear liquids for 1 to 3 days before the test. Examples of clear liquids are: fat-free bouillon or broth, water, clean coffee or tea, strained fruit juices, sports drinks, and gelatin.
Unless otherwise instructed, patients should continue taking any regularly
prescribed medication but stop taking iron preparations a few weeks before
the test, unless otherwise instructed. Iron residues produce a dark black
stool, which makes the view inside the bowel less clear.
People with some heart valve diseases may receive antibiotics before and after the test to prevent infection.
Outpatients must plan to have someone take them home after the test, because
they will be woozy and unable to drive.
How the test feels
The sedative and pain medication are administered to cause relaxation and drowsiness. Many patients do not remember having the colonoscopy. A rectal examination usually is done before the test to widen (dilate) the rectum and make sure there are no major obstructions. An urge to defecate is normal when the rectal exam is performed or as the colonoscope is inserted.
Pressure may be felt as the scope moves inside, and brief cramping and gas pains as air is inserted or the scope advances. Passing gas is necessary and should be expected. Discomfort can be reduced by taking slow, deep breaths. This will also help relax the abdominal muscles. Mild abdominal cramping and considerable passing of gas may occur after the exam. Sedation should wear off in a few hours. Because of the sedation, patients may not feel any discomfort and may have no memory of the test.
Why the test is performed
Colonoscopy may be used for the following reasons:
What abnormal results may indicate
Additional conditions under which the test may be performed:
Risks


