long QT syndrome
Credit: Ion Channel Lab, University of Utah.
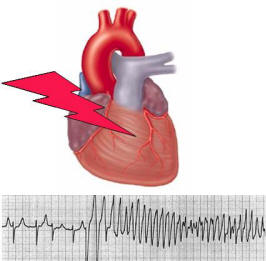
Long QT syndrome (LQTS), also known as Jervell and Lange-Nielsen syndrome and Romano-Ward syndrome, is a disorder of the heart's electrical activity that may cause you to develop a sudden, uncontrollable arrhythmia (abnormal heart rhythm) in response to exercise or stress. Such abnormal heart rhythms also can develop for no known reason in people who have LQTS. Not everyone who has LQTS develops a dangerous heart rhythm, but if one does occur, it may be fatal.
The term "long QT" refers to an abnormality seen on an electrocardiogram (EKG). An EKG is a test that detects and records the electrical activity of the heart. The QT interval, recorded on the EKG, corresponds to the time during which the lower chambers of your heart (the ventricles) are triggered to contract and then build the potential to contract again.
The timing of the electrical activity of the heartbeat is complex and carefully controlled by the body. Normally the QT interval of the heartbeat lasts about a third of each heartbeat cycle on the EKG. But in people with LQTS, the QT interval usually lasts longer than normal, which can upset the careful timing of the heartbeat and trigger a dangerous, irregular rhythm.
Overview
On the surface of each muscle cell in the heart are tiny pores called ion channels. Ion channels open and close to let electrically charged sodium, calcium, and potassium atoms (ions) flow into and out of the cell. This generates the electrical activity of the heart.
This activity causes each heart cell to contract. Normally, the electrical activity spreads from one heart cell to the next in an orderly and coordinated way to allow the heart to pump blood. During each normal heartbeat, the muscle cells in the upper chambers of the heart, the atria, contract. The contraction pumps blood from the atria to the ventricles. Then the muscle cells in the ventricles contract, pumping blood from the ventricles to the lungs and the rest of the body. This coordinated contraction of the atria and ventricles represents one normal heartbeat.
In people who have LQTS, problems with the ion channels in the heart cells may disrupt the timing of the electrical activity in the ventricles. The ion channels may not work properly, or there may be too few of them. In this situation, the heart may suddenly develop a fast and abnormal heart rhythm that can be life threatening.
Many cases of LQTS are inherited, which means you are born with the condition and have it your whole life. There are seven known types of inherited LQTS. The most common ones are called LQTS 1, LQTS 2, and LQTS 3.
Emotional stress or physical exercise (especially swimming) that makes the heart beat faster tends to trigger irregular heart rhythms if you have LQTS 1. In LQTS 2, irregular rhythms may be triggered by surprise or other extreme emotions. In LQTS 3, a low heart rate during sleep may be the trigger for an irregular heart rhythm.
Acquired, or noninherited, LQTS may be brought on by certain medicines and other medical conditions.
Outlook
More than half the people who have an untreated, inherited form of LQTS die within 10 years. But for many people with LQTS, lifestyle changes and medical treatments can help prevent dangerous complications and lengthen life expectancy. Some of these changes include:
Discuss with your doctor the lifestyle changes and treatments that are appropriate for you and the type of LQTS you have.
Causes
Inherited long QT syndrome
Faulty genes that control the production of certain types of ion channels in your heart cells cause inherited long QT syndrome (LQTS). These LQTS genes may cause the body to produce too few ion channels or ion channels that don't work as they should, or both.
If you have inherited LQTS, you received the faulty gene(s) from one or both of your parents. Inherited LQTS is a lifelong condition.
There are seven known types of inherited LQTS (types 1 though 7). The most common types of inherited LQTS are types 1, 2, and 3. Some LQTS types stem from faulty or lacking potassium ion channels, while others are due to faulty or lacking sodium channels.
If you have LQTS 1 and LQTS 2, the flow of potassium ions through the ion channels in your heart cells isn't normal, which may cause problems when you exercise or when you're surprised or experience emotional stress. During these situations, you may develop a rapid and uncontrollable heart rhythm that may prevent your heart from pumping blood. This will result in death if it's not quickly brought under control.
If you have LQTS 3, the flow of sodium ions through ion channels in your heart cells isn't normal, which also may trigger a rapid and uncontrollable heart rhythm that can result in death. In LQTS 3, problems usually develop when your heart beats slower than normal, such as during sleep.
Noninherited long QT syndrome
Acquired, or noninherited, LQTS may be brought on by certain medicines and other medical conditions. Side effects from certain medicines are the most common cause of noninherited LQTS.
Medication-induced long QT syndrome
Presently, more than 50 medicines have been recognized to cause LQTS. Some of the commonly used medicines that may cause LQTS include:
Some people with medication-induced LQTS may also have an inherited form of the syndrome that doesn't cause symptoms unless they take certain medicines that lengthen the QT interval or lower potassium levels in the blood. This is sometimes called silent LQTS.
Other causes of acquired long QT syndrome
Excessive diarrhea or vomiting that causes a major loss of potassium or sodium ions from the bloodstream may cause LQTS. The syndrome lasts until the levels of these ions in the blood return to normal. The eating disorder anorexia nervosa and certain thyroid disorders may cause a drop in potassium ion levels in the blood, causing LQTS.
Who is at risk?
Populations affected
Long QT syndrome is a rare condition. Experts suspect that about 1 in 7,000 people has LQTS. But no one knows for sure, because LQTS often goes undiagnosed.
LQTS causes about 3,000 to 4,000 sudden deaths in children and young adults each year in the United States. Unexplained sudden death in children is rare. But when it does occur, LQTS often is the cause.
Inherited LQTS usually is first detected during childhood or young adulthood. Half of all people with LQTS experience their first irregular heartbeat by the time they're 12 years old, and 90 percent by the time they reach 40 years old. Rarely is inherited LQTS first diagnosed in someone after age 40. In boys with LQTS, the QT interval often returns toward normal after puberty, and the risk of fainting and sudden cardiac arrest decreases.
LQTS is more common in women than men. Women who have LQTS are more likely to experience fainting or sudden death from the condition during menstruation and shortly after giving birth. LQTS also is common in children born deaf. This is because the same genetic abnormality that affects hearing also affects the working of ion channels in the heart.
Major risk factors
You're at risk for having LQTS if anyone in your family has ever had it. Unexplained fainting or seizures, drowning or near drowning, or unexplained sudden death are all possible signs of LQTS.
You're also at risk for LQTS if you take medicines that make the QT interval (on your EKG) longer. Your doctor can tell you whether the medicines you take might do this. You also may develop LQTS if you have excessive vomiting or diarrhea or other conditions that cause low blood levels of potassium or sodium. These conditions include the eating disorder anorexia nervosa and certain thyroid disorders.
Signs and symptoms
Major signs and symptoms
If you have long QT syndrome (LQTS), you're prone to developing a sudden and dangerous arrhythmia. Symptoms or signs of the arrhythmias that people with LQTS tend to have often first appear during childhood and include:
Other signs and symptoms
Often people with LQTS 3 will develop an irregular heartbeat during sleep. This may cause them to have noisy gasping while sleeping.
Diagnosis
Doctors' considerations
Doctors called cardiologists diagnose and treat long QT syndrome (LQTS). Cardiologists are doctors who specialize in treating problems and diseases of the heart. To diagnose LQTS, doctors consider:
EKG
An EKG is a simple test that detects and records the electrical activity of the heart. This test may reveal a long QT interval and other signs that make it more likely that you have LQTS. Often your doctor first discovers you have a long QT interval when an EKG is done for another suspected heart problem.
Not all people with LQTS will always have a long QT interval on an EKG. The QT interval may change from time to time, sometimes being long and other times normal. Because of this, your doctor may want you to have several EKG tests over a period of days or weeks. Or your doctor will have you wear a device called a Holter monitor.
A Holter monitor, also called an ambulatory EKG, records the electrical activity of your heart for a full 24-hour period. For this test, you wear patches called electrodes on your chest that are connected by wires to a small, portable recorder. The recorder may be clipped to a belt, kept in a pocket, or hung around your neck. During the 24 hours, you do your usual daily activities. You then return the recorder to the doctor to read the results. The purpose of a Holter monitor EKG is to detect heart problems that may occur for only a few minutes out of the day.
Some people will only have a long QT interval on an EKG recording while they exercise. For this reason, your doctor may recommend that you have an exercise stress test.
For this test, a machine records your EKG while you exercise. If you're unable to exercise, a medicine may be injected through an intravenous line into your bloodstream to make your heart work harder and beat faster as if you were exercising.
Medical history and physical exam
Your doctor will ask whether you have had any symptoms of an irregular heartbeat. These include:
Your doctor will ask what over-the-counter, prescription, or recreational drugs you take.
Your doctor also will want to know whether anyone in your family was diagnosed with or shows signs of LQTS. Signs of LQTS include unexplained fainting or seizures, drowning, sudden cardiac arrest, or sudden death.
Your doctor will examine you and will look for the presence of conditions that may lower blood levels of potassium or sodium. These conditions include the eating disorder anorexia nervosa, excess vomiting or diarrhea, and certain thyroid disorders.
Genetic tests
Genetic blood tests can detect some forms of inherited LQTS. If your doctor suspects that you have LQTS, he or she may recommend genetic testing. Genetic blood tests are usually also suggested for family members of people with LQTS. But about one-third of LQTS cases aren't detected with genetic testing. Even if you do have LQTS, the tests may not show it.
Also, as many as one-third of the people who test positive for LQTS don't have any signs or symptoms of the disorder. These people may have silent LQTS. Fewer than 1 out of 10 of these people will faint or suddenly die from an irregular heartbeat.
But even if you have silent LQTS, you may be more at risk than most people for developing an irregular heartbeat while taking medicines that affect potassium ion channels or blood levels of potassium.
Types of inherited LQTS
If you have inherited LQTS, it may be helpful to know which of the seven inherited types of the syndrome you have. That way, you and your doctor can better target the treatment and lifestyle measures you need to take. To figure out your LQTS type, your doctor will consider:
Treatment
Goals of treatment
The goal of treating long QT syndrome (LQTS) is to prevent life-threatening, irregular heartbeats and fainting spells. Treatment isn't a cure for this condition and may not restore a long QT interval (on your EKG) to normal. But it does greatly improve survival.
Specific types of treatment
Your doctor will recommend the best treatment for you based on:
People who have a lower risk of complications from LQTS may want to try less aggressive treatments, such as making lifestyle changes (avoiding situations that trigger irregular heartbeats) or taking medicines. The type of LQTS you have will determine which medicines you take to avoid abnormal heart rhythms. For example, doctors will usually only prescribe sodium channel blocker medicines for people with LQTS 3.
If your doctor thinks you're at higher risk for complications from your LQTS, he or she may recommend other more aggressive treatments (in addition to medicines and lifestyle changes). Such aggressive treatments include:
Patients at higher risk are those who have fainted or who have developed dangerous heart rhythms from their LQTS in the past.
Lifestyle changes
If you have LQTS, you should try to avoid, if possible, the specific triggers you have for an irregular heartbeat. Many people with LQTS also benefit from adding more potassium to their diets. They should check with their doctor about eating more potassium-rich foods, such as bananas, or taking potassium supplements daily.
People with LQTS also should avoid medicines that lengthen the QT interval or lower potassium blood levels. (See "What Causes Long QT Syndrome?")
Medicines
Beta blocker heart medicines prevent the heart from beating faster in response to physical or emotional stress. Most people with LQTS are treated with beta blockers. Doctors may suggest that people with LQTS 3 take sodium channel blocker medicines, such as mexiletine. These make sodium ion channels less active.
Pacemaker or implantable cardioverter defibrillator
These are surgically implanted devices that monitor the heart rhythm and deliver electrical currents to the heart when they detect an abnormal heart rhythm. Surgeons implant pacemakers and ICDs in the chest or belly with a minor procedure.
Surgery
People at high risk of death from LQTS are sometimes treated with surgery in which the nerves that prompt the heart to beat faster in response to physical or emotional stress are cut. This helps to keep the heart beating at a steady pace and decreases the chances of developing dangerous heart rhythms in response to stress or exercise.
Living with long QT syndrome
Long QT syndrome is usually a lifelong condition. The risk of developing an irregular heartbeat that leads to fainting or sudden cardiac arrest may lessen as you age, but the risk never disappears. You need to take certain steps for the rest of your life to prevent an irregular heartbeat or to ensure that you get immediate treatment if one occurs. These steps include:
Avoid triggers
If exercise triggers an irregular heartbeat, your doctor may recommend that you avoid any strenuous exercise, especially swimming. Ask your doctor which types of exercise are right for you. If you have a pacemaker or implantable cardioverter defibrillator you will need to avoid contact sports that may dislodge these devices. You may want to only exercise in public or with a friend who will help you if you faint.
Avoid medicines that may trigger an irregular heartbeat. These medicines include those used to treat allergies, infections, high blood pressure, high cholesterol, and depression. Consult with your doctor before you take any prescription, over-the-counter, or other drugs.
Seek medical care immediately for conditions that lower the potassium level in your blood. These conditions include excessive diarrhea, vomiting, or the eating disorder anorexia nervosa.
Avoid unexpected noises in your bedroom if you have LQTS 2. These noises include loud or jarring alarm clock buzzers and telephone ringers.
Inform others
You may want to consider wearing a medical identification bracelet that states that you have LQTS. Let your roommates, coworkers, or other people with whom you have regular contact know that you have a condition that might cause you to faint or your heart to stop beating. Let these people know that they should get you emergency medical care immediately if you faint.
You may want to have someone in your family or office learn cardiopulmonary resuscitation (CPR) in case your heart stops beating. You also could keep an automatic external defibrillator with you at home or at work. This device uses electrical shocks to restore your heartbeat to normal. Someone at your home or work should be trained how to use the device if your heart stops beating.
If you have LQTS 3 and you sleep alone, you may want to have an intercom in your bedroom connected to someone else's bedroom. This will let others detect the noisy gasping that often occurs if you develop an irregular heartbeat while lying down.
Ongoing health care needs
You should see your cardiologist regularly. He or she will adjust your treatment as needed. For example, if you still faint often while using less aggressive treatments, your doctor may recommend other options to better prevent the abnormal heart rhythms you're having.
It can be stressful to have LQTS, or to have a family member with it. You may want to ask your doctor to recommend a LQTS support group.


