atrial fibrillation
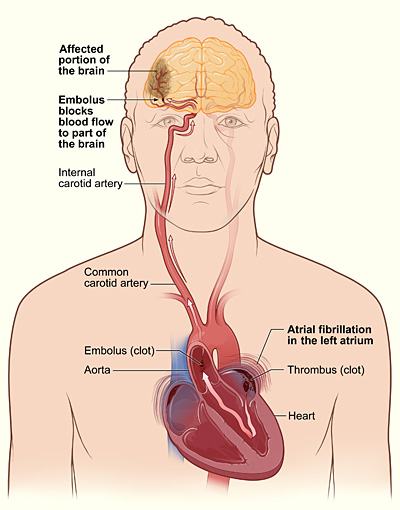
The illustration shows how a stroke can occur during atrial fibrillation. If a clot (thrombus) forms in the left atrium of the heart, a piece of it can dislodge and travel to an artery in the brain, blocking blood flow through the artery. The lack of blood flow to the portion of the brain fed by the artery causes a stroke.
Atrial fibrillation, or AF, is the most common arrhythmia. An arrhythmia is a problem with the speed or rhythm of the heartbeat. A disorder in the electrical system of the heart causes AF and other types of arrhythmia.
AF occurs when rapid, disorganized electrical signals in the heart's two upper chambers, called the atria, cause them to contract very fast and irregularly (this is called fibrillation). As a result, blood pools in the atria and isn't pumped completely into the heart's two lower chambers, called the ventricles. When this happens, the heart's upper and lower chambers don't work together as they should.
Often, people who have AF may not even feel symptoms. However, even when not noticed, AF can lead to an increased risk of stroke. In many patients, particularly when the rhythm is extremely rapid, AF can cause chest pain, heart attack, or heart failure. AF may occur rarely or every now and then, or it may become a persistent or permanent heart rhythm lasting for years.
Understanding the heart's electrical system
The heart has an internal electrical system that controls the speed and rhythm of the heartbeat. With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As it travels, the signal causes the heart to contract and pump blood. The process repeats with each new heartbeat.
Each electrical signal begins in a group of cells called the sinus node, or sinoatrial (SA) node. The SA node is located in the right atrium, which is the upper right chamber of the heart. In a healthy adult heart at rest, the SA node fires off an electrical signal to begin a new heartbeat 60 to 100 times a minute. (This rate may be slower in very fit athletes.)
From the SA node, the electrical signal travels through special pathways to the right and left atria. This causes the atria to contract and pump blood into the heart's two lower chambers, the ventricles. The electrical signal then moves down to a group of cells called the atrioventricular (AV) node, located between the atria and the ventricles. Here, the signal slows down just a little, allowing the ventricles time to finish filling with blood.
The electrical signal then leaves the AV node and travels along a pathway called the bundle of His. This pathway divides into a right bundle branch and a left bundle branch. The signal goes down these branches to the ventricles, causing them to contract and pump blood out to the lungs and the rest of the body. The ventricles then relax, and the heartbeat process starts all over again in the SA node.
Understanding the electrical problem in atrial fibrillation
In AF, the heart's electrical signal begins in a different part of the atria or the nearby pulmonary veins and is conducted abnormally. The signal doesn't travel through normal pathways, but may spread throughout the atria in a rapid, disorganized way. This can cause the atria to beat more than 300 times a minute in a chaotic fashion. The atria's rapid, irregular, and uncoordinated beating is called fibrillation.
The abnormal signal from the SA node floods the AV node with electrical impulses. As a result, the ventricles also begin to beat very fast. However, the AV node can't conduct the signals to the ventricles as fast as they arrive, so even though the ventricles may be beating faster than normal, they aren't beating as fast as the atria. The atria and ventricles no longer beat in a coordinated fashion, creating a fast and irregular heart rhythm. In AF, the ventricles may beat up to 100–175 times a minute, in contrast to the normal rate of 60–100 beats a minute.
When this happens, blood isn't pumped into the ventricles as well as it should be, and the amount of blood pumped out of the ventricles is based on the randomness of the atrial beats. In AF, instead of the body receiving a constant, regular amount of blood from the ventricles, it receives rapid, small amounts and occasional random, larger amounts, depending on how much blood has flowed from the atria to the ventricles with each beat.
Most of the symptoms of AF are related to how fast the heart is beating. If medicines or age slow the heart rate, the effect of the irregular beats is minimized.
AF may be brief, with symptoms that come and go and end on their own, or it may be persistent and require treatment. Or, AF can be permanent, in which case medicines or other interventions can't restore a normal rhythm.
Outlook
People who have AF can live normal, active lives. For some people, treatment can cure AF and return their heartbeat to a normal rhythm. For people who have permanent AF, treatment can successfully control symptoms and prevent complications. Treatment consists primarily of different kinds of medicines or nonsurgical procedures.
Types of atrial fibrillation
Paroxysmal atrial fibrillation
In paroxysmal atrial fibrillation (AF), the abnormal electrical signals and rapid heart rate begin suddenly and then stop on their own. Symptoms can be mild or severe and last for seconds, minutes, hours, or days.
Persistent atrial fibrillation
Persistent AF is a condition in which the abnormal heart rhythm continues until it is stopped with treatment.
Permanent atrial fibrillation
Permanent AF is a condition in which the normal heart rhythm can't be restored with the usual treatments. Both paroxysmal and persistent atrial fibrillation may become more frequent and eventually result in permanent AF.
Causes
Atrial fibrillation (AF) occurs when the electrical signals traveling through the heart are conducted abnormally and become disorganized and very rapid.
This is the result of damage to the heart's electrical system. This damage is most often the result of other conditions, such as coronary artery disease or high blood pressure, that affect the health of the heart. Sometimes, the cause of AF is unknown.
Who is at risk?
Populations affected
More than 2 million people in the United States have atrial fibrillation (AF), and it affects both men and women. AF generally occurs in older people, mostly because they're more likely to have heart disease or conditions that increase the risk of AF. AF is uncommon among young people.
Major risk factors
AF is more common in people with heart diseases or conditions, including:
AF also is more common in people who are having a heart attack or who have just had surgery.
Other conditions that increase AF risk include hyperthyroidism, obesity, high blood pressure (hypertension), diabetes, and lung diseases.
Recent evidence suggests that patients who receive high-dose steroid therapy are at increased risk of AF. This therapy, which is commonly used for asthma and certain inflammatory conditions, may act as a trigger in people who already have other risk factors for AF.
Signs and symptoms
Atrial fibrillation (AF) usually causes the ventricles to contract faster than normal. When this happens, the ventricles don't have enough time to fill completely with blood to pump to the lungs and body. This inefficient pumping can cause signs and symptoms, such as:
Complications
AF has two major complications – stroke and heart failure. Heart attack is another, rarer complication.
Stroke
During AF, the atria don't pump all of their blood to the ventricles. Some blood pools in the atria. When this happens, a blood clot (also called a thrombus) can form. If the clot breaks off and travels to the brain, it can cause a stroke. (A clot that forms in one part of the body and travels in the bloodstream to another part of the body is called an embolus.)
Blood-thinning medicines to reduce the risk of stroke are a very important part of treatment for patients who have AF.
Heart failure
Heart failure occurs when the heart can't pump enough blood to meet the body's needs. Because the ventricles are beating very fast and aren't able to properly fill with blood to pump out to the body, AF can lead to heart failure.
Fatigue and shortness of breath are common symptoms of heart failure. A buildup of fluid in the lungs causes these symptoms. Fluid also can build up in the feet, ankles, and legs, causing weight gain.
Lifestyle changes, medicines, and sometimes special care (rarely, a mechanical heart pump or heart transplant) are the main treatments for heart failure.
Diagnosis
Sometimes people have atrial fibrillation (AF), but don't have symptoms. For these people, AF is often found during a physical exam or electrocardiogram (EKG) test done for another purpose. Other times, AF is diagnosed after a person goes to the doctor because of symptoms.
To understand why a person has AF and the best way to treat it, the doctor will want to discover any immediate or underlying causes. Doctors use several methods to diagnose AF, including family and medical history, a physical exam, and several diagnostic tests and procedures.
Specialists involved
A primary care doctor often is involved in the initial diagnosis and treatment of AF. These doctors can include:
Doctors who specialize in the diagnosis and treatment of heart disease also may be involved, such as:
Family and medical history
The doctor will ask questions about:
Physical exam
The doctor will do a complete cardiac exam, listening to the rate and rhythm of your heartbeat and taking your pulse and blood pressure reading. The doctor will likely check to see whether you have any sign of problems with your heart muscle or valves. He or she will listen to your lungs to check for signs of heart failure.
The doctor also will check for swelling in the legs or feet and look for an enlarged thyroid gland or other signs of hyperthyroidism.
Diagnostic tests and procedures
EKG
An EKG is a simple test that detects and records the electrical activity of your heart. It is the most useful test for diagnosing AF. It shows how fast the heart is beating and its rhythm (steady or irregular). It also records the timing of the electrical signals as they pass through each part of the heart.
A standard EKG test only records the heartbeat for a few seconds. It won't detect an AF episode that doesn't happen during the test. To diagnose paroxysmal AF, the doctor may ask you to wear a portable EKG monitor that can record your heartbeat for longer periods. The two most common types of portable EKGs are Holter and event monitors.
Holter monitor
Also called an ambulatory EKG, this device records the electrical signals of the heart for a full 24- or 48-hour period. You wear small patches called electrodes on your chest that are connected by wires to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
During the time you're wearing a Holter monitor, you do your usual daily activities and keep a notebook, noting any symptoms you have and the time they occurred. You then return both the recorder and the notebook to the doctor to read the results. The doctor can see how your heart was beating at the time you had symptoms.
Event monitor
Event monitors are useful to diagnose AF that occurs only once in a while. The device is worn continuously, but only records the heart's electrical activity when you push a button. You push the button on the device when you feel symptoms. Event monitors can be worn for 1 to 2 months, or as long as it takes to get a recording of the heart when symptoms are occurring.
Other tests used to diagnose atrial fibrillation
Echocardiogram
This test uses sound waves to create a moving picture of your heart. An echocardiogram provides information about the size and shape of your heart and how well your heart chambers and valves are functioning. The test also can identify areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
This test is sometimes called a transthoracic echocardiogram. It is noninvasive and is done by placing an echo probe on your chest wall. The procedure is the same technique used for obtaining sonograms in pregnant women.
Transesophageal echocardiogram
A transesophageal echocardiogram, or TEE, takes pictures of the heart through your esophagus (the tube leading from your mouth to your stomach). The atria are deep in the chest and often can't be seen very well on a regular echocardiogram. A doctor can see the atria much better with a TEE. In this test, the transducer is attached to the end of a flexible tube that's guided down your throat and into your esophagus. TEE is usually done while the patient under some sedation. TEE is used to detect clots that may be developing in the atria because of AF.
Blood tests
Blood tests check the level of thyroid hormone and the balance of your body's electrolytes. Electrolytes are minerals in your blood and body fluids that are essential for normal health and functioning of your body's cells and organs.
Treatment
Treatment for atrial fibrillation (AF) depends on how severe or frequent the symptoms are and whether you already have heart disease. General treatment options include medicines, medical procedures, and lifestyle changes.
Goals of treatment
Treatment of AF is designed to:
Who needs treatment for atrial fibrillation?
People with no symptoms and no related heart problems may not need treatment. AF may even go back to a permanent normal heart rhythm on its own. In some people who have AF for the first time, doctors may choose to use an electrical procedure or medicine to restore the heart rhythm to normal.
Repeated episodes of AF tend to cause changes to the electrical system of the heart, leading to persistent or permanent AF. Most people with persistent or permanent AF need treatment to control their heart rate and prevent complications.
Specific types of treatment
Blood clot prevention
The risk of a blood clot traveling from the heart to the brain and causing a stroke is increased in people who have AF. Preventing the formation of blood clots is probably the most important part of treating AF. Doctors prescribe blood-thinning medicines to prevent blood clots. These medicines include warfarin (Coumadin®), heparin, and aspirin.
Warfarin is the most effective medicine in people with risk factors for stroke. People taking warfarin must have regular blood tests to check how well the medicine is working.
Rate control
Doctors also prescribe medicines to slow down the rate at which the ventricles are beating. These medicines help bring the heart rate to a normal level.
Rate control is the recommended strategy for most patients with AF, even though the heart rhythm continues to be abnormal and the heart doesn't work as efficiently as it could. Most people feel better and can function well if their heart rate is well controlled.
Medicines used to control the heart rate include beta blockers (for example, metoprolol and atenolol), calcium channel blockers (diltiazem and verapamil), and digoxin. Several other medicines also are available.
Rhythm control
Doctors use medicines or procedures to restore and maintain the heart's rhythm. This treatment approach is recommended for people who aren't functioning well with rate control treatment or who have only recently started having AF.
The longer you have AF, the less likely it is that an abnormal heart rhythm can be restored to a normal heart rhythm. This is especially true for people who have had AF for 6 months or more.
Restoring a normal rhythm also becomes less likely if the atria become enlarged or if any underlying heart disease becomes more severe. In these situations, the chance that AF will recur is high, even if you're taking a medicine to help convert AF to a normal rhythm.
Medicines
Medicines used to control a person's heart rhythm include amiodarone, sotalol, flecainide, propafenone, dofetilide, ibutilide, and occasionally older medicines such as quinidine, procainamide, and disopyramide.
Medicines must be carefully tailored to the person taking them because they can cause a different kind of irregular, slow, or rapid heartbeat (arrhythmia) or can be harmful in people who have underlying diseases of the heart or other organs. This is particularly true for those patients who have an unusual heart rhythm problem called Wolff-Parkinson-White syndrome.
To convert AF to a normal heart rhythm, people can be given AF medicines regularly by injection at a doctors office, clinic, or hospital. Or, to try to control AF or prevent recurrences, people may take pills on an ongoing basis. If the doctor knows how a person will react to a medicine, a specific dose may be prescribed according to the "pill in the pocket" technique. This means that a patient takes a specific dose of a medicine as needed only if he or she has an episode of AF, but not on a regular, daily basis.
Procedures
Doctors use several procedures to restore a normal heart rhythm, including:
Before doing electrical cardioversion, the doctor may recommend a transesophageal echocardiogram (TEE) to rule out the presence of blood clots in the atria. If clots are present, the patient may need to receive blood-thinning medicines to help eliminate the clots before the electrical cardioversion.
Approaches to treating underlying causes and reducing risk factors
The doctor also may suggest other approaches designed to treat the underlying condition that may be causing AF or to reduce risk factors for AF. These approaches include prescribing medicines to treat an overactive thyroid, reduce blood pressure and overweight, or treat other underlying causes of AF.
The doctor also may recommended lifestyle changes, such as reducing stress, quitting smoking, reducing salt intake (to help lower blood pressure), and eating healthily. Limiting or avoiding stress as well as alcohol, caffeine, or other stimulants that may increase your heart rate also may help to reduce the risk of AF.
Prevention
You may be able to prevent atrial fibrillation (AF) by leading a healthy lifestyle and taking steps to lower your risk for heart disease. These steps include:
If you have heart disease or risk factors, you should work with your doctor to control your condition and lower your risk of complications, such as AF. In addition to following the healthy lifestyle steps above, which also can help control heart disease, your doctor may advise you to to take one or more of the following steps:
Living with atrial fibrillation
People who have atrial fibrillation (AF) – even permanent AF – can live normal, active lives.
If you have AF, you should:


