thoracentesis
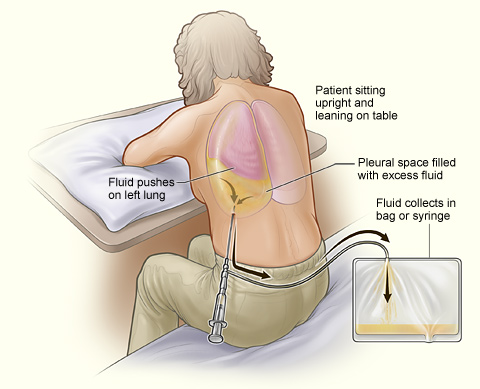
A person having thoracentesis. The person sits upright and leans on a table. Excess fluid from the pleural space is drained into a bag.
Thoracentesis is a procedure to remove excess fluid in the space between the lungs and the chest wall. This space is called the pleural space.
Normally, the pleural space is filled with a small amount of fluid – about 4 teaspoons full. But some conditions, such as heart failure, lung infections, and tumors, can cause more fluid to build up. When this happens, it's called a pleural effusion. A lot of extra fluid can press on the lungs, making it hard to breathe.
Overview
Thoracentesis is done to find the cause of a pleural effusion. It also may be done to help you breathe easier.
During the procedure, your doctor inserts a thin needle or plastic tube into the pleural space and draws out the excess fluid. Usually, doctors take only the amount of fluid needed to find the cause of the pleural effusion. However, if there's a lot of fluid, they may take more. This helps the lungs expand and take in more air, which allows you to breathe easier.
After the fluid is removed from your chest, it's sent for testing. Once the cause of the pleural effusion is known, your doctor will plan treatment. For example, if an infection is causing the excess fluid, you may be given antibiotics to fight the infection. If the cause is heart failure, you will be treated for that condition.
Thoracentesis usually takes 10 to 15 minutes. It may take longer if there's a lot of fluid in the pleural space. You will be watched for up to a few hours after the procedure for complications.
Outlook
The procedure usually doesn't cause serious problems, but some risks are involved. These include pneumothorax, or collapsed lung; pain, bleeding, bruising, or infection where the needle or tube was inserted; and liver or spleen injury (very rare).
Most of these complications get better on their own, or they're easily treated.
Who needs thoracentesis?
You may need thoracentesis if you have a pleural effusion. A pleural effusion is the buildup of excess fluid in the pleural space (the space between the lungs and chest wall).
Thoracentesis helps find the cause of the pleural effusion. It also may be done to help you breathe easier, if there's a lot of fluid in the pleural space.
The most common cause of a pleural effusion is heart failure. This is a condition in which the heart can't pump enough blood to the body.
Other causes include lung cancer, tumors, pneumonia, tuberculosis, pulmonary embolism, and other lung infections. Asbestosis, sarcoidosis, and reactions to some drugs also can lead to a pleural effusion.
Diagnosing a pleural effusion
A pleural effusion is diagnosed based on your medical history, a physical exam, and test results.
Medical history
Your doctor will ask about your symptoms, like trouble breathing, coughing, and hiccups. Other things your doctor may ask about include whether you've ever:
Physical exam
Your doctor will listen to your breathing with a stethoscope and tap lightly on your chest. If you have a pleural effusion, your breathing may sound muffled. There also may be a dull sound when your doctor taps on your chest.
Diagnostic tests
Your doctor may use one or more of the following tests to diagnose a pleural effusion.
Before thoracentesis
Before thoracentesis, your doctor will talk to you about the procedure and how to prepare for it. Tell your doctor what medicines you're taking, about any previous bleeding problems, and about allergies to medicines or latex.
No special preparations are needed before thoracentesis.
During thoracentesis
Thoracentesis is done at a doctor's office or hospital. The entire procedure (including preparation) usually takes 10 to 15 minutes, but the needle or tube is in your chest for only a few minutes during that time. If there's a lot of fluid, the procedure may take up to 45 minutes.
You will sit on the edge of a chair or exam table, lean forward, and rest your arms on a table. Your doctor will tell you not to move, cough, or breathe deeply once the procedure begins.
He or she cleans the area of your skin where the needle or tube will be inserted and injects medicine to numb the area. You may feel some stinging at this time.
Your doctor then inserts the needle or tube between your ribs and into the pleural space (the area between the lungs and chest wall). You may feel some discomfort and pressure at this time. Your doctor may use ultrasound to find the right place to insert the needle or tube. (Ultrasound uses sound waves to create images of your lungs.)
He or she then draws out the excess fluid around your lungs using the needle or tube. You may feel like coughing, and you may feel some chest pain. If a lot of fluid is removed, your lungs will have more room to fill with air as the fluid is drawn out. This can make it easier to breathe.
Once the fluid is removed, your doctor takes out the needle or tube. A small bandage is placed on the site where the needle or tube was inserted.
After thoracentesis
After thoracentesis, you may need a chest X-ray to check for any lung problems. Your blood pressure and breathing will be checked for up to a few hours to make sure you don't have complications.
Your doctor will let you know when you can return to your normal activities, such as driving, physical activity, and working.
Once at home, call your doctor right away if you have any breathing problems.
What thoracentesis shows
Your doctor will send the fluid removed during thoracentesis for testing. It will be looked at for signs of heart failure, infection, cancer, or other conditions that may be causing the pleural effusion (the buildup of fluid between the lungs and chest wall).
Once the cause of the pleural effusion is known, your doctor will talk to you about a treatment plan. For example, if an infection is causing the excess fluid, you may need antibiotics to fight the infection. If the cause is heart failure, you will be treated for that condition.
Risks
The risks of thoracentesis are usually minor and will get better on their own, or they're easily treated. Your doctor may do a chest X-ray after the procedure to check for lung problems.
The risks of thoracentesis include:


