myasthenia gravis
The faces of people who suffer from Myasthenia gravis often having a sagging appearance. Hence, M.G. is sometimes called "Rag Doll" syndrome. Image credit: M. G. Association, UK.
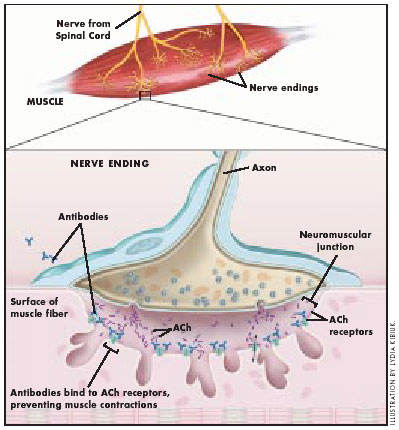
Myasthenia gravis occurs when the immune system makes antibodies that damage or block many of the muscle's acetylcholine (ACh) receptors on the surface of muscle cells. This prevents ACh from binding to the damaged receptors and acting on the muscle, which reduces muscle contractions, leading to weakness and fatigue. Image: Lydia Kibiuk.
Myasthenia gravis is a chronic autoimmune neuromuscular disease (see autoimmune disease) characterized by varying degrees of weakness of the skeletal (voluntary) muscles of the body. The name myasthenia gravis, which is Latin and Greek in origin, literally means "serious muscle weakness." With current therapies, however, most cases of myasthenia gravis are not as serious as the name implies. In fact, for the majority of individuals with myasthenia gravis, life expectancy is not lessened by the disorder.
The hallmark of myasthenia gravis is muscle weakness that increases during periods of activity and improves after periods of rest. Certain muscles such as those that control eye and eyelid movement, facial expression, chewing, talking, and swallowing are often, but not always, involved in the disorder. The muscles that control breathing and neck and limb movements may also be affected.
Causes
Myasthenia gravis is caused by a defect in the transmission of nerve impulses to muscles. It occurs when normal communication between the nerve and muscle is interrupted at the neuromuscular junction – the place where nerve cells connect with the muscles they control. Normally when impulses travel down the nerve, the nerve endings release a neurotransmitter substance called acetylcholine. Acetylcholine travels through the neuromuscular junction and binds to acetylcholine receptors which are activated and generate a muscle contraction.
In myasthenia gravis, antibodies block, alter, or destroy the receptors for acetylcholine at the neuromuscular junction which prevents the muscle contraction from occurring. These antibodies are produced by the body's own immune system. Thus, myasthenia gravis is an autoimmune disease because the immune system – which normally protects the body from foreign organisms – mistakenly attacks itself.
Role of thymus gland in myasthenia gravis
The thymus gland, which lies in the upper chest area beneath the sternum (breastbone), plays an important role in the development of the immune system in early life. Its cells form a part of the body's normal immune system. The gland is somewhat large in infants, grows gradually until puberty, and then gets smaller and is replaced by fat with age. In adults with myasthenia gravis, the thymus gland is abnormal. It contains certain clusters of immune cells indicative of lymphoid hyperplasia – a condition usually found only in the spleen and lymph nodes during an active immune response. Some individuals with myasthenia gravis develop thymomas or tumors of the thymus gland. Generally thymomas are benign, but they can become malignant.
The relationship between the thymus gland and myasthenia gravis is not yet fully understood. Scientists believe the thymus gland may give incorrect instructions to developing immune cells, ultimately resulting in autoimmunity and the production of the acetylcholine receptor antibodies, thereby setting the stage for the attack on neuromuscular transmission.
Symptoms
Although myasthenia gravis may affect any voluntary muscle, muscles that control eye and eyelid movement, facial expression, and swallowing are most frequently affected. The onset of the disorder may be sudden. Symptoms often are not immediately recognized as myasthenia gravis.
In most cases, the first noticeable symptom is weakness of the eye muscles. In others, difficulty in swallowing and slurred speech may be the first signs. The degree of muscle weakness involved in myasthenia gravis varies greatly among patients, ranging from a localized form, limited to eye muscles (ocular myasthenia), to a severe or generalized form in which many muscles – sometimes including those that control breathing – are affected. Symptoms, which vary in type and severity, may include a drooping of one or both eyelids (ptosis), blurred or double vision (diplopia) due to weakness of the muscles that control eye movements, unstable or waddling gait, weakness in arms, hands, fingers, legs, and neck, a change in facial expression, difficulty in swallowing and shortness of breath, and impaired speech (dysarthria).
Who gets myasthenia gravis?
Myasthenia gravis occurs in all ethnic groups and both genders. It most commonly affects young adult women (under 40) and older men (over 60), but it can occur at any age.
In neonatal myasthenia, the fetus may acquire immune proteins (antibodies) from a mother affected with myasthenia gravis. Generally, cases of neonatal myasthenia gravis are transient (temporary) and the child's symptoms usually disappear within 2-3 months after birth. Other children develop myasthenia gravis indistinguishable from adults. Myasthenia gravis in juveniles is common.
Myasthenia gravis is not directly inherited nor is it contagious. Occasionally, the disease may occur in more than one member of the same family.
Rarely, children may show signs of congenital myasthenia or congenital myasthenic syndrome. These are not autoimmune disorders, but are caused by defective genes that produce proteins in the acetylcholine receptor or in acetylcholinesterase.
Diagnosis
Unfortunately, a delay in diagnosis of one or two years is not unusual in cases of myasthenia gravis. Because weakness is a common symptom of many other disorders, the diagnosis is often missed in people who experience mild weakness or in those individuals whose weakness is restricted to only a few muscles.
The first steps of diagnosing myasthenia gravis include a review of the individual's medical history, and physical and neurological examinations. The signs a physician must look for are impairment of eye movements or muscle weakness without any changes in the individual's ability to feel things. If the doctor suspects myasthenia gravis, several tests are available to confirm the diagnosis.
A special blood test can detect the presence of immune molecules or acetylcholine receptor antibodies. Most patients with myasthenia gravis have abnormally elevated levels of these antibodies. However, antibodies may not be detected in patients with only ocular forms of the disease.
Another test is called the edrophonium test. This approach requires the intravenous administration of edrophonium chloride or Tensilon, a drug that blocks the degradation (breakdown) of acetylcholine and temporarily increases the levels of acetylcholine at the neuromuscular junction. In people with myasthenia gravis involving the eye muscles, edrophonium chloride will briefly relieve weakness. Other methods to confirm the diagnosis include a version of nerve conduction study which tests for specific muscle "fatigue" by repetitive nerve stimulation. This test records weakening muscle responses when the nerves are repetitively stimulated. Repetitive stimulation of a nerve during a nerve conduction study may demonstrate decrements of the muscle action potential due to impaired nerve-to-muscle transmission.
A different test called single fiber electromyography (EMG), in which single muscle fibers are stimulated by electrical impulses, can also detect impaired nerve-to-muscle transmission. EMG measures the electrical potential of muscle cells. Muscle fibers in myasthenia gravis, as well as other neuromuscular disorders, do not respond as well to repeated electrical stimulation compared to muscles from normal individuals. Computed tomography (CT) may be used to identify an abnormal thymus gland or the presence of a thymoma.
A special examination called pulmonary function testing - which measures breathing strength - helps to predict whether respiration may fail and lead to a myasthenic crisis.
Treatment
Today, myasthenia gravis can be controlled. There are several therapies available to help reduce and improve muscle weakness. Medications used to treat the disorder include anticholinesterase agents such as neostigmine and pyridostigmine, which help improve neuromuscular transmission and increase muscle strength. Immunosuppressive drugs such as prednisone, cyclosporine, and azathioprine may also be used. These medications improve muscle strength by suppressing the production of abnormal antibodies. They must be used with careful medical follow-up because they may cause major side effects.
Thymectomy, the surgical removal of the thymus gland (which often is abnormal in myasthenia gravis patients), reduces symptoms in more than 70 percent of patients without thymoma and may cure some individuals, possibly by re-balancing the immune system. Other therapies used to treat myasthenia gravis include plasmapheresis, a procedure in which abnormal antibodies are removed from the blood, and high-dose intravenous immune globulin, which temporarily modifies the immune system and provides the body with normal antibodies from donated blood. These therapies may be used to help individuals during especially difficult periods of weakness. A neurologist will determine which treatment option is best for each individual depending on the severity of the weakness, which muscles are affected, and the individual's age and other associated medical problems.
What are myasthenic crises?
A myasthenic crisis occurs when the muscles that control breathing weaken to the point that ventilation is inadequate, creating a medical emergency and requiring a respirator for assisted ventilation. In patients whose respiratory muscles are weak, crises – which generally call for immediate medical attention – may be triggered by infection, fever, or an adverse reaction to medication.
Prognosis
With treatment, the outlook for most patients with myasthenia gravis is bright: they will have significant improvement of their muscle weakness and they can expect to lead normal or nearly normal lives. Some cases of myasthenia gravis may go into remission temporarily and muscle weakness may disappear completely so that medications can be discontinued. Stable, long-lasting complete remissions are the goal of thymectomy. In a few cases, the severe weakness of myasthenia gravis may cause a crisis (respiratory failure), which requires immediate emergency medical care. (see above).
Research
Much has been learned about myasthenia gravis in recent years. Technological advances have led to more timely and accurate diagnosis, and new and enhanced therapies have improved management of the disorder. Much knowledge has been gained about the structure and function of the neuromuscular junction, the fundamental aspects of the thymus gland and of autoimmunity, and the disorder itself. Despite these advances, however, there is still much to learn. The ultimate goal of myasthenia gravis research is to increase scientific understanding of the disorder. Researchers are seeking to learn what causes the autoimmune response in myasthenia gravis, and to better define the relationship between the thymus gland and myasthenia gravis.
Today's myasthenia gravis research includes a broad spectrum of studies conducted and supported by NINDS. NINDS scientists are evaluating new and improving current treatments for the disorder. One such study is testing the efficacy of intravenous immune globlin in patients with myasthenia gravis. The goal of the study is to determine whether this treatment safely improves muscle strength. Another study seeks further understanding of the molecular basis of synaptic transmission in the nervous system. The objective of this study is to expand current knowledge of the function of receptors and to apply this knowledge to the treatment of myasthenia gravis.


