thrombotic thrombocytopenic purpura
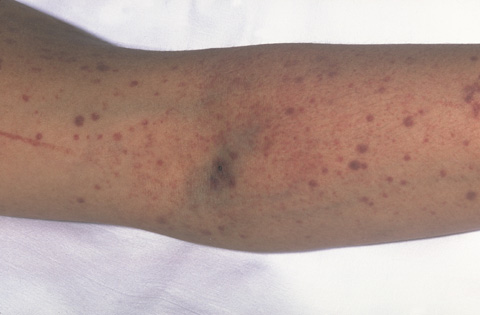
Purpura.
Thrombotic thrombocytopenic purpura (TTP) is a rare blood condition. It causes blood clots to form in small blood vessels throughout the body. These blood clots can cause serious problems if they block blood vessels and limit blood flow to the brain, kidneys, or heart.
Blood clots form when blood cells called platelets clump together. Platelets are made in your bone marrow along with other kinds of blood cells. They stick together to seal small cuts or breaks and stop bleeding.
In TTP, when blood clots form, there are fewer platelets in the blood. This can cause bleeding into the skin (purpura), prolonged bleeding from cuts, and internal bleeding. It also causes small blood clots to form suddenly throughout the body, including in the brain and kidneys.
Thrombotic refers to the blood clots that form. Thrombocytopenic means there's a lower than normal number of platelets in the blood. Purpura are purple bruises caused by bleeding into the skin.
TTP also can cause red blood cells to break apart faster than the body can replace them. This leads to hemolytic anemia – a rare form of anemia. Anemia is a condition in which a person's blood doesn't have enough red blood cells.
A lack of activity in the ADAMTS13 enzyme (a type of protein in the blood) causes TTP. The ADAMTS13 gene controls the enzyme, which is involved in blood clotting. The enzyme breaks up a large protein called von Willebrand factor that clumps together with platelets to form blood clots.
Types of thrombotic thrombocytopenic purpura
TTP has two main types: inherited and acquired (noninherited) TTP.
Inherited means the condition is passed from parents to children. This type
of TTP mainly affects newborns and children. In inherited TTP, the ADAMTS13
gene is faulty and doesn't prompt the body to make a normal ADAMTS13 enzyme.
As a result, enzyme activity is lacking or is changed.
Acquired TTP is the more common type. Acquired means you aren't born with the condition, but you develop it. This type of TTP occurs mostly in adults, but it sometimes affects children.
In acquired TTP, the ADAMTS13 gene isn't changed. Instead, the body makes proteins called antibodies that block the ADAMTS13 enzyme's activity.
What triggers inherited and acquired TTP isn't known, but some factors may play a role. These include:
Outlook
TTP is a rare condition. It can be fatal or cause lasting damage, such as brain damage or stroke, if it's not treated right away. About 1,200 people develop acquired TTP each year in the United States.
TTP usually occurs suddenly and lasts for days and weeks, but it can continue for months. Most people recover fully from TTP when treated promptly. Relapses (or flareups) can occur in 30 to 60 percent of people with acquired TTP. Many people with inherited TTP have frequent flareups that need to be treated.
Treatments for TTP include infusions of fresh frozen plasma and plasma exchange (also called plasmapheresis). These treatments have greatly improved the outlook of the disease.
Causes
A lack of activity in the ADAMTS13 enzyme causes thrombotic thrombocytopenic purpura (TPP). The ADAMTS13 gene controls the enzyme, which is involved in blood clotting.
Not having enough enzyme activity causes platelets to clump together, forming blood clots. In TTP, when blood clots form, there are fewer platelets in the blood. This can cause bleeding into the skin (purpura), drawn-out bleeding from cuts, and internal bleeding. It also causes small blood clots to form suddenly throughout the body, including in the brain and kidneys.
TTP also can cause red blood cells to break apart faster than the body can replace them. This leads to hemolytic anemia.
Inherited thrombotic thrombocytopenic purpura
In the inherited form of TTP, changes in the ADAMTS13 gene affect the enzyme's function. The gene doesn't prompt the body to make a normal ADAMTS13 enzyme. As a result, enzyme activity is lacking or is altered.
In inherited TTP, a person is born with two copies of the altered gene – one from each parent. Most often, the parents each have one copy of the altered gene, but have no signs or symptoms of the disorder.
Acquired thrombotic thrombocytopenic purpura
In the acquired type of TTP, the ADAMTS13 gene isn't changed. Instead, the body makes proteins called antibodies that block the ADAMTS13 enzyme's activity.
Triggers for thrombotic thrombocytopenic purpura
What triggers TTP isn't known, but some factors may play a role. These include:
Who is at risk?
Thrombotic thrombocytopenic purpura (TTP) is a rare condition. About 1,200 new cases occur each year in the United States.
Most cases of TTP are the acquired type. Acquired TTP mostly occurs in adults, but it can affect children. The condition is seen more often in women than in men.
Inherited TTP mainly affects newborns and children. Most people who have inherited TTP begin to have symptoms soon after birth. Some, however, don't have their first episode of disease until they're adults.
Signs and symptoms
Signs and symptoms of thrombotic thrombocytopenic purpura (TTP) are due to blood clots, a low platelet count, and damaged red blood cells.
The signs and symptoms include:
If you've had TTP and have any of these signs and symptoms, call your doctor right away.
Diagnosis
Your doctor will diagnosis thrombotic thrombocytopenic purpura (TTP) based on your medical history, a physical exam, and test results.
If TTP is suspected or diagnosed, a hematologist (a doctor who specializes in blood diseases) will be involved in your care.
Medical history
Your doctor will ask about factors that may affect TTP, such as:
Physical exam
Your doctor will do a physical exam and look for signs such as:
Diagnostic tests
Your doctor also may order tests to help find out if you have TTP.
Complete blood count
This test measures the number of red and white blood cells and platelets in your blood. For this test, a small amount of blood is drawn from a vein (blood vessel), usually in your arm.
If you have TTP, your platelet count will be low and you will have a lower than normal number of red blood cells (anemia).
Blood smear
For this test, a small amount of blood is drawn from a vein, usually in your arm. Some of your blood is put on a glass slide. A microscope is then used to look at your red blood cells. In TTP, the red blood cells are torn and broken.
Platelet count
This test counts the number of platelets in a blood smear. People with TTP have a lower than normal number of platelets in their blood. This test is used with the blood smear to help diagnose TTP.
Bilirubin test
When red blood cells die, they release a protein called hemoglobin into the bloodstream. The body breaks down hemoglobin into a compound called bilirubin. High levels of bilirubin in the bloodstream cause jaundice.
For this blood test, a small amount of blood is drawn from a vein, usually in your arm. In TTP, bilirubin may be high because your body is breaking down red blood cells at a faster than normal rate.
Kidney function tests and urine tests
These tests are done to see whether your kidneys are working well. In TTP, your urine may contain protein or blood cells. Also your blood creatinine level may be high. Creatinine is a blood product that normally is removed by the kidneys.
Coombs test
This blood test is used to see whether TTP is the cause of hemolytic anemia. For this test, a small amount of blood is drawn from a vein, usually in your arm.
In TTP, hemolytic anemia occurs when red blood cells are broken into pieces as they try to squeeze around blood clots.
When TTP is the cause of hemolytic anemia, the Coombs test is negative. It's positive when antibodies that bind to red blood cells cause your immune system to destroy the cells.
Lactate dehydrogenase test
This blood test measures a protein called lactate dehydrogenase (LDH). For this test, a small amount of blood is drawn from a vein, usually in your arm.
Hemolytic anemia causes red blood cells to break and release this protein into the blood. LDH also is released from tissues that are injured by blood clots as a result of TTP.
ADAMTS13 assay
A lack of activity of the ADAMTS13 enzyme causes TTP. For this test, a small amount of blood is drawn from a vein, usually in your arm. The blood is sent to a special lab to test for the enzyme's activity.
Treatment
Thrombotic thrombocytopenic purpura (TTP) can be fatal or cause lasting damage, such as brain damage or stroke, if it's not treated promptly.
In most cases, TTP occurs suddenly and lasts for days and weeks, but it can go on for months. Most people recover fully when treated right away. Relapses (flareups) can occur in 30 to 60 percent of people with acquired TTP. Flareups also occur in most people with inherited TTP.
Plasma treatments are the most common way to treat TTP. Other treatments include medicines and surgery. Treatments are done in a hospital.
Plasma therapy
Plasma is the liquid part of your blood. It carries blood cells, hormones, enzymes, and nutrients to your body.
TTP is treated with plasma therapy. This includes fresh frozen plasma for newborns and children with inherited TTP, and plasma exchange for people with acquired TTP. Plasma therapy is started in the hospital as soon as TTP is diagnosed or suspected.
For inherited TTP, fresh frozen plasma is given through an intravenous (IV) line in a vein (blood vessel). This is done to replace the missing or changed ADAMTS13 enzyme.
For acquired TTP, plasma exchange (also called plasmapheresis) is done. This is a lifesaving procedure. It removes antibodies from the blood that damage your ADAMTS13 enzyme. It also replaces the ADAMTS13 enzyme. If plasma exchange isn't available, you may be given fresh frozen plasma until it is available.
During plasma exchange, an IV needle or tube is placed in your arm to remove blood. The blood then goes through a cell separator, which removes plasma from the blood. The nonplasma part of the blood is saved, and donated plasma is added to it.
The blood is then put back into you through an IV line in one of your blood vessels. The time the procedure takes varies, but it often takes about 2 hours.
Treatments of fresh frozen plasma or plasma exchange usually continue until your blood tests and signs and symptoms improve. This can be days or weeks depending on your condition. You will stay in the hospital during this time.
Some people who recover from TTP have flareups. This can happen in the hospital or after you go home. If you have a flareup, plasma infusion or plasma exchange will be restarted.
Other treatments
Other treatments are used when plasma infusions or plasma exchange doesn't work well or when flareups occur often.
Medicines are used to slow or stop antibodies from forming. In acquired TTP, antibodies block the activity of the ADAMTS13 enzyme. Medicines used to treat TTP include glucocorticoids, vincristine, rituximab, and cyclosporine A.
Surgery to remove the spleen (an organ in the abdomen) is sometimes needed. This is because cells in the spleen make antibodies that block the activity of the ADAMTS13 enzyme.
Prevention
Both inherited and acquired thrombotic thrombocytopenic purpura (TTP) appear suddenly with no clear cause. You can't prevent either type. If you've had TTP, it's important to watch for signs and symptoms of a relapse (flareup).
You also should talk to your doctor about factors that may trigger TTP or a flareup, including:
Living with thalassemia
Most people recover fully from thrombotic thrombocytopenic purpura (TTP) when treated promptly. Relapses (or flareups) can occur in 30 to 60 percent of cases.
If this happens, plasma therapy and/or medicines will need to be restarted.
If you've had TTP, you should call your doctor right away if you have signs or symptoms of a relapse. These signs and symptoms include:
If you have been successfully treated for TTP, you should talk to your doctor about using any medicines – such as aspirin and ibuprofen – that can raise your risk of bleeding during a relapse. Also, tell your doctor about all over-the-counter medicines you take, including vitamins, supplements, or herbal remedies.
If your child has inherited TTP, ask the doctor whether you need to restrict your child's activities.
Report any symptoms of infection, such as a fever, to your doctor. This is very important for people who have had their spleens removed.
Talk to your doctor about changing medicines that may raise your risk for TTP, such as ticlopidine and clopidogrel.


