aneurysm

Figure 1. Aneurysms come in two general shapes. The first is called a saccular aneurysm and is a formation of a sac or pouch on one side of the blood vessel wall. The second type is called a fusiform aneurysm and is an outward bulging of the blood vessel wall in all directions. A ruptured aneurysm is one that has burst and caused bleeding into the surrounding tissues.
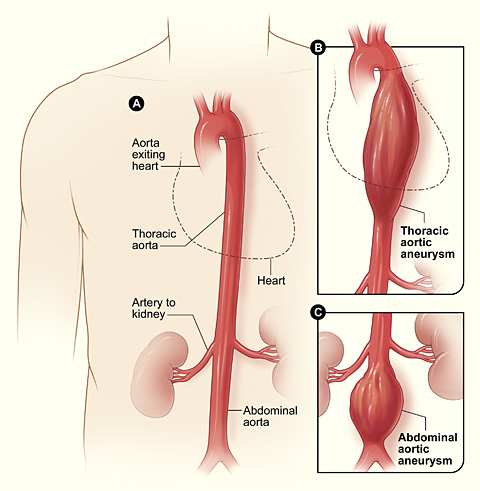
Figure 2. Diagram A shows a normal aorta. Diagram B shows a thoracic aortic aneurysm located behind the heart. Diagram C shows an abdominal aortic aneurysm located below the arteries that supply the kidneys.
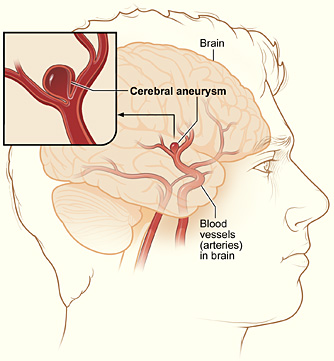
Figure 3. Typical location of a cerebral (berry) aneurysm in the arteries supplying blood to the brain. The inset image shows a close-up of the sac-like aneurysm.
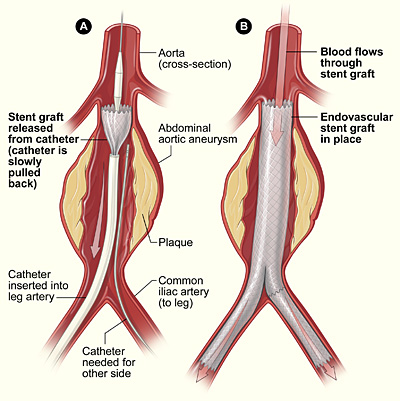
Figure 4. Placement of an endovascular stent graft in an aortic aneurysm. In figure A, a catheter is inserted into an artery in the groin (upper thigh). It is then threaded up to the abdominal aorta, and the stent graft is released from the catheter. In figure B, the stent graft allows blood to flow through the aneurysm.
An aneurysm is an abnormal bulge or ballooning (dilation) in the wall of an artery caused by the pressure of blood flowing through a weakened area. The weakening may be the result of disease, injury, or a congenital defect of the arterial wall.
Arteries are blood vessels that carry oxygen-rich blood from the heart to other parts of the body. An aneurysm that grows and becomes large enough can burst, causing dangerous, often fatal, bleeding inside the body.
Most aneurysms occur in the aorta – the main artery that carries blood from the heart to the rest of the body (Figure 2). The aorta emerges from the left ventricle of the heart and travels through the chest and abdomen. An aneurysm that occurs in the aorta in the chest is called a thoracic aortic aneurysm. An aneurysm that occurs in the aorta in the abdomen is called an abdominal aortic aneurysm.
Aneurysms also can occur in arteries in the brain, heart, intestine, neck, spleen, back of the knees and thighs, and in other parts of the body. If an aneurysm in the brain bursts, it causes a stroke.
In the United States alone, about 15,000 people die each year from ruptured aortic aneurysms. In fact, ruptured aortic aneurysm is the tenth leading cause of death in men over age 50 in the US.
Many cases of ruptured aneurysm can be prevented with early diagnosis and medical treatment. Because aneurysms can develop and become large before causing any symptoms, it is important to look for them in people who are at the highest risk. Experts recommend that men who are 65 to 75 years old and have ever smoked (at least 100 cigarettes in their lifetime) should be checked for abdominal aortic aneurysms.
When found in time, aneurysms can usually be treated successfully with medicines or surgery. If an aortic aneurysm is found, the doctor may prescribe medicine to reduce the heart rate and blood pressure. This can reduce the risk of rupture.
Large aortic aneurysms, if found in time, can often be repaired with surgery to replace the diseased portion of the aorta. The outlook is usually excellent.
Types of aneurysm
Types of aneurysm include aortic aneurysms, cerebral aneurysms, and peripheral aneurysms.
Aortic aneurysm
Most aneurysms occur in the aorta. The two types of aortic aneurysm are thoracic aortic aneurysm (TAA) and abdominal aortic aneurysm (AAA).
Thoracic aortic aneurysm
An aortic aneurysm that occurs in the part of the aorta running through the thorax (chest) is a thoracic aortic aneurysm. One in four aortic aneurysms is a TAA. Most TAAs do not produce symptoms, even when they are large. Only half of all people with TAAs notice any symptoms. TAAs are identified more often now than in the past because of chest computed tomography (CT) scans performed for other medical problems.
In a common type of TAA, the walls of the aorta become weak and a section nearest to the heart enlarges. Then the valve between the heart and the aorta cannot close properly and blood leaks backward into the heart. Less commonly, a TAA can develop in the upper back away from the heart. A TAA in this location can result from and injury to the chest such as from an auto crash.
Abdominal aortic aneurysm
An aortic aneurysm that occurs in the part of the aorta running through the abdomen is an abdominal aortic aneurysm. Three in four aortic aneurysms are AAAs. An AAA can grow very large without producing symptoms. About 1 in 5 AAAs rupture.
Cerebral aneurysm
Aneurysms that occur in an artery in the brain are called cerebral aneurysms (Figure 3). They are sometimes called berry aneurysms because they are often the size of a small berry. Most cerebral aneurysms produce no symptoms until they become large, begin to leak blood, or rupture.
A ruptured cerebral aneurysm causes a stroke. Signs and symptoms can include a sudden, extremely severe headache, nausea, vomiting, stiff neck, sudden weakness in an area of the body, sudden difficulty speaking, and even loss of consciousness, coma, or death. The danger of a cerebral aneurysm depends on its size and location in the brain, whether it leaks or ruptures, and the person's age and overall health.
Peripheral aneurysm
Aneurysms that occur in arteries other than the aorta (and not in the brain) are called peripheral aneurysms. Common locations for peripheral aneurysms include the artery that runs down the back of the thigh behind the knee (the popliteal artery), the main artery in the groin (the femoral artery), and the main artery in the neck (the carotid artery).
Peripheral aneurysms are not as likely to rupture as aortic aneurysms, but blood clots can form in peripheral aneurysms. If a blood clot breaks away from the aneurysm, it can block blood flow through the artery. If a peripheral aneurysm is large, it can press on a nearby nerve or vein and cause pain, numbness, or swelling.
Who is at risk?
Populations affected
Men are 5 to 10 times more likely than women to have an abdominal aortic aneurysm (AAA) – the most common type of aneurysm.
The risk of AAA increases with age, and is more likely to occur in people between the ages of 60 to 80. A peripheral aneurysm also is more likely to affect people ages 60 to 80. Cerebral (brain) aneurysms, though rare, are more likely to occur in people ages 35 to 60.
Risk factors
Factors that increase the risk for aneurysm include:
Untreated syphilis (a very rare cause today)
Tuberculosis (also a very rare cause today)
Signs and symptoms
The signs and symptoms of an aneurysm depend on its type, location, and whether it has ruptured or is interfering with other structures in the body. Aneurysms can develop and grow for years without causing any signs or symptoms. It is often not until an aneurysm ruptures or grows large enough to press on nearby parts of the body or block blood flow that it produces any signs or symptoms.
Abdominal aortic aneurysm
Most abdominal aortic aneurysms (AAAs) develop slowly over years and have no signs or symptoms until (or if) they rupture. Sometimes, a doctor can feel a pulsating mass while examining a patient's abdomen. When symptoms are present, they can include:
If an AAA ruptures, symptoms can include sudden, severe pain in the lower abdomen and back; nausea and vomiting; clammy, sweaty skin; lightheadedness; and a rapid heart rate when standing up. Internal bleeding from a ruptured AAA can send you into shock. Shock is a life-threatening condition in which the organs of the body do not get enough blood flow.
Thoracic aortic aneurysm
A thoracic (chest) aortic aneurysm may have no symptoms until the aneurysm begins to leak or grow. Signs or symptoms may include:
Cerebral aneurysm
If a cerebral (brain) aneurysm presses on nerves in the brain, it can cause signs and symptoms. These can include:
If a cerebral aneurysm ruptures, symptoms can include a sudden, severe headache, nausea and vomiting, stiff neck, loss of consciousness, and signs of a stroke. Signs of a stroke are similar to those listed above for cerebral aneurysm, but they usually come on suddenly and are more severe. Any of these symptoms require immediate medical attention.
Peripheral aneurysm
Signs and symptoms of peripheral aneurysm may include:
An aneurysm in the popliteal artery (behind the knee) can compress nerves and cause pain, weakness, and numbness in the knee and leg.
Blood clots can form in peripheral aneurysms. If a clot breaks loose and travels through the bloodstream, it can lodge in the arm, leg, or brain and block the artery. An aneurysm in the neck can block the artery to the brain and cause a stroke.
Diagnosis
An aneurysm may be found by chance during a routine physical exam. More often, an aneurysm is found by chance during an X-ray, ultrasound, or computed tomography (CT) scan performed for another reason, such as chest or abdominal pain.
If an abdominal aortic aneurysm (AAA) is present, it may be felt as a pulsating mass in the abdomen. A rapidly growing aneurysm about to rupture can be tender and very painful when pressed. In someone who is overweight or obese, it may be difficult for a doctor to feel even a large abdominal aneurysm.
If an AAA is present, a doctor may hear rushing blood flow instead of the normal whooshing sound when listening to the abdomen with a stethoscope.
Specialists involved
Patients may be referred to a cardiothoracic surgeon, vascular surgeon, or neurosurgeon for diagnosis and treatment of an aneurysm. A cardiothoracic surgeon performs surgery on the heart, lungs, and other organs and structures in the chest, including the aorta. A vascular surgeon performs surgery on the abdominal aorta and on the peripheral arteries. A neurosurgeon performs surgery on the brain, including the arteries in the head, and on the spine and nerves.
Diagnostic tests and procedures
To diagnose and evaluate an aneurysm, one or more of the following tests or procedures may be performed:
Treatment
Some aneurysms, mainly small ones that are not causing pain, can be treated with "watchful waiting." Others need to be treated to prevent growth and complications. The goals of treatment are to prevent the aneurysm from growing, prevent or reverse damage to other body structures, prevent or treat a rupture, and to allow the patient to continue to participate in normal daily activities.
Treatment options
Medicine and surgery are the two types of treatment for an aneurysm. Medicines may be prescribed before surgery or instead of surgery. Medicines are used to reduce pressure, relax blood vessels, and reduce the risk of rupture. Beta blockers and calcium channel blockers are the medicines most commonly used.
Surgery may be recommended if an aneurysm is large and likely to rupture.
Treatment by type of aneurysm
Aortic aneurysm
Experts recommend that men who have ever smoked (at least 100 cigarettes in their lifetime) and are between the ages of 65 and 75 should have an ultrasound screening to check for abdominal aortic aneurysms.
Treatment recommendations for aortic aneurysms are based on the size of the aneurysm. Small aneurysms found early can be treated with "watchful waiting."
Two main types of surgery to repair aortic aneurysms are open abdominal or open chest repair and endovascular repair.
The traditional and most common type of surgery for aortic aneurysms is open abdominal or open chest repair. It involves a major incision in the abdomen or chest. General anesthesia is needed with this procedure.
The aneurysm is removed and the section of aorta is replaced with an artificial graft made of material such as Dacron® or Teflon®. The surgery takes 3 to 6 hours, and the patient remains in the hospital for 5 to 8 days. It often takes a month to recover from open abdominal or open chest surgery and return to full activity. Open abdominal and chest surgeries have been performed for 50 years. More than 90 percent of patients make a full recovery.
In endovascular repair (see Fig 4), the aneurysm is not removed, but a graft is inserted into the aorta to strengthen it. This type of surgery is performed through catheters (tubes) inserted into the arteries; it does not require surgically opening the chest or abdomen.
To perform endovascular repair, the doctor first inserts a catheter into an artery in the groin (upper thigh) and threads it up to the area of the aneurysm. Then, watching on X-ray, the surgeon threads the graft (also called a stent graft) into the aorta to the aneurysm. The graft is then expanded inside the aorta and fastened in place to form a stable channel for blood flow. The graft reinforces the weakened section of the aorta to prevent the aneurysm from rupturing.
Endovascular repair surgery reduces recovery time to a few days and greatly reduces time in the hospital. The procedure has been used since 1999. Not all aortic aneurysms can be repaired with this procedure. The exact location or size of the aneurysm may prevent the stent graft from being safely or reliably positioned inside the aneurysm.
Cerebral aneurysm
Treatment for cerebral (brain) aneurysms depends on the size and location of the aneurysm, whether it is infected, and whether it has ruptured. A small cerebral aneurysm that hasn't burst may not need treatment. A large cerebral aneurysm may press against brain tissue, causing a severe headache or impaired vision, and is likely to burst. If the aneurysm ruptures, there will be bleeding into the brain which will cause a stroke. If a cerebral aneurysm becomes infected, it requires immediate medical treatment. Treatment of many cerebral aneurysms, especially large or growing ones, involves surgery, which can be risky depending on the location of the aneurysm.
Peripheral aneurysm
Most peripheral aneurysms have no symptoms, especially if they are small. They seldom rupture.
Treatment of peripheral aneurysms depends on the presence of symptoms, the location of the aneurysm, and whether the blood flow through the artery is blocked. Blood clots can form in a peripheral aneurysm, break loose, and block the artery.
An aneurysm in the back of the knee that is larger than 1 inch in diameter usually requires surgery. An aneurysm in the thigh also is usually repaired with surgery.
Prevention
The best way to prevent an aneurysm is to avoid the risk factors that increase the changes of developing one. To do this, a person can:


