A heart attack, also known as myocardial infarction or coronary thrombosis, occurs when the supply of blood and oxygen to an area of heart
muscle is blocked, usually by a clot in a coronary
artery. Often, this blockage leads to arrhythmias (irregular heartbeat or rhythm) that cause a severe decrease in the pumping
function of the heart and may bring about
sudden death. If the blockage is not treated within a few hours, the affected
heart muscle will die and be replaced by scar tissue.
A heart attack is a life-threatening event. Everyone should know the warning
signs of a heart attack and how to get emergency help. Many people suffer
permanent damage to their hearts or die because they do not get help immediately.
Each year, more than a million persons in the US have a heart attack and
about half (515,000) of them die. About one-half of those who die do so
within 1 hour of the start of symptoms and before reaching the hospital.
Emergency personnel can often stop arrhythmias with emergency CPR (cardiopulmonary
resuscitation), defibrillation (electrical shock), and prompt advanced cardiac
life support procedures. If care is sought soon enough, blood flow in the
blocked artery can be restored in time to
prevent permanent damage to the heart. Yet, most people do not seek medical
care for 2 hr or more after symptoms begin. Many people wait 12 hr
or longer.
A heart attack is an emergency. Prompt treatment of a heart attack can help
prevent or limit lasting damage to the heart and can prevent sudden death.
Causes
Most heart attacks are caused by a blood clot that blocks one of the coronary
arteries (the blood vessels that bring blood and oxygen to the heart muscle).
When blood cannot reach part of your heart, that area starves for oxygen.
If the blockage continues long enough, cells in the affected area die.
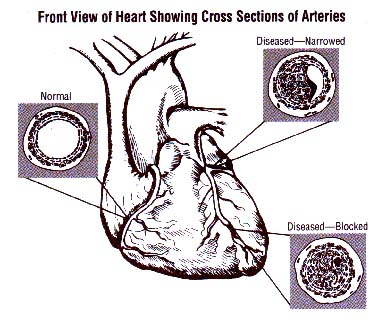
Coronary artery disease (CAD) is the most common underlying cause of a heart attack. CAD is the
hardening and narrowing of the coronary arteries by the buildup of plaque in the inside walls (atherosclerosis).
Over time, plaque buildup in the coronary arteries can:
Narrow the arteries so that less blood flows to the heart muscle
Completely block the arteries and the flow of blood
Cause blood clots to form and block the arteries.
A less common cause of heart attacks is a severe spasm (tightening) of the
coronary artery that cuts off blood flow to the heart. These spasms can
occur in persons with or without CAD. Artery spasm can sometimes be caused
by:
Taking certain drugs, such as cocaine
Emotional stress
Exposure to cold
Cigarette smoking.
What makes a heart attack more likely
Certain factors make it more likely that you will develop CAD and have a
heart attack. These are called risk factors. Risk factors you cannot change
include:
Your age
- Men: over age 45
- Women: over age 55
Having a family history of early heart disease
- Heart disease diagnosed in father or brother before age 55
- Heart disease diagnosed in mother or sister before age 65
Having a personal history of CAD
-
Angina
- A previous heart attack
- A surgical procedure (
angioplasty,
heart bypass) to increase blood flow to your heart.
Risk factors that you can change include:
Smoking
High blood pressure
High blood cholesterol
Obesity
Being physically inactive
Diabetes (high blood
sugar).
Signs and symptoms
The warning signs and symptoms of a heart attack can include:
Chest discomfort. Most heart attacks involve discomfort in the center
of the chest that lasts for more than a few minutes, or goes away and
comes back. The discomfort can feel like uncomfortable pressure, squeezing,
fullness, or pain. Heart attack pain can sometimes feel like indigestion
or heartburn.
Discomfort in other areas of the upper body. Can include pain, discomfort,
or numbness in one or both arms, the back, neck, jaw, or stomach.
Shortness of breath. Often comes along with chest discomfort. But
it also can occur before chest discomfort.
Other symptoms. May include breaking out in a cold sweat, having nausea and vomiting, or feeling light-headed
or dizzy.
Signs and symptoms vary from person to person. In fact, if you have a second
heart attack, your symptoms may not be the same as for the first heart attack.
Some people have no symptoms. This is called a "silent" heart attack.
The symptoms of angina can be similar to
those of a heart attack. If you have angina and notice a change or a worsening
of your symptoms, talk with your doctor right away.
Diagnosis
Diagnosis (and treatment) of a heart attack can begin when emergency medical
personnel arrive.
At the hospital emergency room, doctors will work fast to find out if you
are having or have had a heart attack. They will consider your symptoms,
medical and family history, and test results. Initial tests will be quickly
followed by treatment if you are having a heart attack.
Tests used include:
Electrocardiogram (ECG or EKG). This test is used to measure the rate and regularity of
your heartbeat. A 12-lead EKG is used in diagnosing a heart attack.
Blood tests. When cells
in the heart die, they release enzymes into the blood. They are called
markers or biomarkers. Measuring the amount of these markers in the
blood can show how much damage was done to your heart. These tests are
often repeated at intervals to check for changes. The specific blood
tests are:
-
Troponin test. This test checks the troponin levels in the
blood. It is considered the most accurate blood test to see if a heart
attack has occurred and how much damage was done to the heart.
-
CK or CK-MB test. These tests check for the amount of the
different forms of creatine
kinase in the blood.
-
Myoglobin test. This test checks for the presence of myoglobin
in the blood. Myoglobin is released when the heart or other muscle
is injured.
Nuclear heart scan. This test uses radioactive tracers (technetium or thallium) to outline heart chambers
and major blood vessels leading to and from the heart. A nuclear heart
scan shows any damage to your heart muscle.
Cardiac catheterization.
A thin flexible tube (catheter) is passed through an artery in the groin
or arm to reach the coronary arteries. Your doctor can determine pressure
and blood flow in the heart's chambers, collect blood samples from the
heart, and examine the arteries of the heart by X-ray.
Coronary angiography.
This test is usually performed along with cardiac catheterization. A
dye that can be seen using X-ray is injected through the catheter into
the coronary arteries. Your doctor can see the flow of blood through
the heart and see where there are blockages.
Treatment
A heart attack is a medical emergency. Delaying treatment can mean lasting
damage to your heart or even death. The sooner treatment begins, the better
your chances of recovering. Your treatment may begin in the ambulance or
in the emergency room and continue in a special area called a coronary care
unit or CCU.
In the hospital
If you are having a heart attack, doctors will:
Work quickly to restore blood flow to the heart
Continuously monitor your vital signs to detect and treat complications
Restoring blood flow to the heart is vital to prevent or limit damage to
the heart muscle and to prevent another heart attack. The main treatments
are the use of thrombolytic ("clot-busting") drugs and procedures such as
angioplasty.
Thrombolytic drugs ("clot-busters") are used to dissolve blood
clots that are blocking blood flow to the heart. When given soon after
a heart attack begins, these drugs can limit or prevent permanent damage
to the heart. To be most effective, they need to be given within 1 hour
after of the start of heart attack symptoms.
Angioplasty procedures
are used to open blocked or narrowed coronary arteries. A stent, which
is a tiny metal mesh tube, may be placed in the artery to help keep
it open.
Coronary artery
bypass surgery uses arteries or veins from other areas in your
body to bypass your blocked coronary arteries.
The CCU is specially equipped with monitors that continuously measure your
vital signs. Those that can show signs of complications include:
EKG, which detects any heart
rhythm (arrhythmia) or functional problems
Blood pressure
Pulse oximetry, which measures
the amount of oxygen in the blood and provides an early warning sign
of a low level of oxygen in the blood.
Medications used in treating heart attacks include:
Beta blockers to decrease
the workload on your heart by slowing your heart
rate. This makes your heart beat with less force and lowers your
blood pressure. Some beta blockers are also used to relieve angina (chest
pain) and in heart attack patients to help prevent additional heart
attacks. They are also used to correct irregular heartbeat.
Angiotensin-converting enzyme (ACE) inhibitors to lower blood pressure and reduce the strain on your
heart. They are used in some patients after a heart attack to increase
survival rate and help slow down further weakening of the heart.
Nitrates, such as nitroglycerin,
to relax blood vessels and stop chest pain.
Anticoagulants to thin
the blood and prevent clots from forming in your arteries.
Antiplatelet medications (such as aspirin and clopidigrel) to stop platelets from clumping together to form clots. These medications are given to
people who have had a heart attack, have angina, or who experience angina
after angioplasty.
Glycoprotein IIb-IIIa inhibitors, which are potent antiplatelet
medicines given intravenously to prevent clots from forming in your
arteries.
Medicines to relieve pain and anxiety.
Medicines to treat arrhythmias (irregular heart rhythms), which often
occur during a heart attack.
Oxygen therapy.
The length of your hospital stay after a heart attack depends on your condition
and response to treatment. Most people spend several days in the hospital
after a heart attack. While in the hospital, your heart will be monitored,
and you will receive needed medications. You will probably have further
testing, and you will be treated for any complications that arise.
While you are still in the hospital or after you go home after your heart
attack, your doctor may order other tests, such as:
Echocardiogram. In this test, ultrasound is used to make
an image of your heart that can be seen on a video monitor. It shows
how well the heart is filling with blood and pumping it to the rest
of the body.
Exercise stress test. This
test shows how well your heart pumps at higher workloads when it needs
more oxygen. EKG and blood pressure readings are taken before, during,
and after exercise to see how your heart responds to exercise. The first
EKG and blood pressure reading are done to get a baseline. Readings
are then taken while you walk on an exercise treadmill or pedal a stationary
bicycle. The test continues until you reach a heart rate set by your
doctor. The exercise part is stopped if chest pain or a very sharp rise
in blood pressure occurs. Monitoring continues for 10 to 15 minutes
after exercise or until your heart rate returns to baseline.
Cardiac rehabilitation
Your doctor may prescribe cardiac rehabilitation (rehab) to help you recover
from a heart attack and help prevent another heart attack. Almost everyone
who has survived a heart attack can benefit from rehab.
The cardiac rehab team may include:
Doctors
Your family doctor
A heart specialist
A surgeon
Nurses
Exercise specialists
Physical therapists and occupational therapists
Dietitians
Psychologists or other behavior therapists.
Rehab has two parts:
Exercise training to help you learn how to exercise safely, strengthen
your muscles, and improve your stamina. Your exercise plan will be based
on your individual ability, needs, and interests.
Education, counseling, and training to help you understand your heart
condition and find ways to reduce your risk of future heart problems.
The cardiac rehab team will help you learn how to cope with the stress
of adjusting to a new lifestyle and to deal with your fears about the
future.
After leaving hospital
After a heart attack, your treatment may include cardiac rehab in the first
weeks or months, checkups and tests, lifestyle changes, and medications.
You will need to see your doctor for checkups and tests to see how your
heart is doing. Your doctor will most likely recommend lifestyle changes,
such as quitting smoking, losing weight, changing your diet, or increasing
your physical activity.
After a heart attack, most people take daily medications. These may include:
Aspirin
Medicines that lower your cholesterol or your blood pressure
Other medicines to help reduce your heart's workload.