oxygen therapy
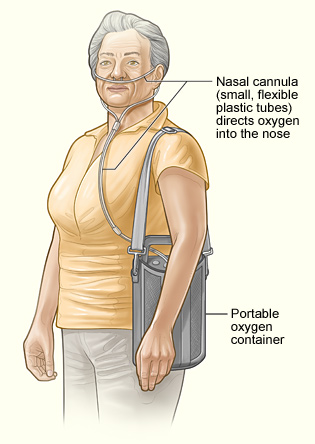
Nasal cannula and portable oxygen container attached to a patient.
Oxygen therapy is a treatment that provides a person with extra oxygen, a gas that the body needs to work properly. Normally, the lungs absorb oxygen from the air. However, some diseases and conditions can prevent the body from getting enough oxygen. Oxygen therapy can help ensure a person gets enough oxygen, which may help him or her function better and be more active.
Oxygen is supplied in a metal cylinder or other container. It flows through a tube and is delivered to your lungs in one of the following ways:
• Through a nasal cannula, which consists of two small plastic tubes, or prongs, that are placed in both nostrils.
• Through a face mask, which fits over your nose and mouth.
• Through a tracheostomy. This is a surgically made hole that goes through the front of your neck and into your windpipe. A breathing tube is placed in the hole to help you breathe. Oxygen delivered this way is called transtracheal oxygen therapy.
Oxygen therapy can be done in a hospital, another medical setting, or at home. If a person needs oxygen therapy for a chronic (ongoing) disease or condition, he or she may receive home oxygen therapy.
Overview
To understand how oxygen therapy works, it helps to understand how your respiratory system works. This system is a group of organs and tissues that help you breathe. It includes the airways and lungs.
The airways are pipes that carry oxygen-rich air to your lungs. They also carry carbon dioxide, a waste gas, out of your lungs.
Air enters your body through your nose or mouth, which moistens and warms the air. The air then travels through your larynx (voice box) and down your trachea (windpipe). The windpipe divides into two tubes called bronchi that enter your lungs.
Within your lungs, your bronchi branch into thousands of smaller, thinner tubes called bronchioles. These tubes end in bunches of tiny round air sacs called alveoli. Each of these air sacs is covered in a mesh of tiny blood vessels called capillaries. The capillaries connect to a network of arteries and veins that move blood through your body.
Oxygen from the air moves through the very thin walls of the alveoli to the surrounding capillaries. The oxygen-rich blood then travels to the heart through the pulmonary vein and its branches. The heart pumps the oxygen-rich blood to your organs.
Certain acute (short-term) and chronic (ongoing) diseases and conditions can affect the transfer of oxygen from the alveoli into the blood. Examples include pneumonia and COPD (chronic obstructive pulmonary disease).
Your doctor will decide whether you need oxygen therapy based on the results of tests, such as an arterial blood gas test and a pulse oximetry test. These tests measure how much oxygen is in your blood. A low level of oxygen is a sign that you need oxygen therapy.
Because oxygen is considered a medicine, your doctor must prescribe it.
Outlook
For many people who get oxygen therapy, the supplemental (extra) oxygen allows them to function better and be more active. Oxygen therapy can help in various ways. It may help:
• Decrease shortness of breath and fatigue
• Improve sleep in some people who have sleep-related breathing disorders
• Increase the lifespan of some people who have COPD
Although you may need oxygen long term, the therapy doesn't have to limit your daily routine. Portable oxygen units can make it easier for you to move around and do many daily activities. Talk with your doctor if you have questions about whether certain activities are safe for you.
A home equipment provider will work with you to make sure you have the supplies and equipment you need. Trained personnel also will show you how to use the equipment correctly and safely.
Oxygen therapy generally is safe, but the oxygen can pose a fire hazard. To use your oxygen safely, follow the instructions you receive from your home equipment provider.
Who needs oxygen therapy?
Your doctor may recommend oxygen therapy if you have a low blood oxygen level. Normally, your lungs absorb oxygen from the air and transfer it into your bloodstream. However, some diseases and conditions can prevent you from getting enough oxygen. These include acute (short-term) and chronic (ongoing) diseases and conditions.
Acute diseases and conditions
You may be given oxygen therapy if you're in the hospital for a serious condition that limits your ability to get enough oxygen. Once you've recovered from the condition, the oxygen likely will be stopped.
Some conditions that may require short-term oxygen therapy are:
• Severe pneumonia. Pneumonia is an infection in one or both of the lungs. In severe cases, the infection causes your lungs' air sacs to become very inflamed. This prevents the air sacs from transferring enough oxygen into your blood.
• Severe asthma attack. Asthma is a lung disease that inflames and narrows the airways. Most people who have asthma, including many children, can safely manage their symptoms. But if you have a severe asthma attack that you can't relieve with your usual treatments, you may need hospital care that includes oxygen therapy.
• Respiratory distress syndrome and/or bronchopulmonary dysplasia in premature babies. Premature babies may develop one or both of these serious lung conditions. As part of their treatment, they may receive extra oxygen from a CPAP (continuous positive airway pressure) machine or a ventilator, or through a tube in the nose.
Chronic diseases and conditions
Certain diseases and conditions may require long-term home oxygen therapy. These diseases and conditions include:
• Chronic obstructive pulmonary disease (COPD). This is a progressive disease in which damage to the air sacs prevents them from transferring enough oxygen into the bloodstream. "Progressive" means the disease gets worse over time.
• Late-stage heart failure. This is a condition in which the heart can't pump enough oxygen-rich blood to meet the body's needs.
• Cystic fibrosis (CF). CF is an inherited disease of the secretory glands, including the glands that make mucus and sweat. People who have CF have thick, sticky mucus that collects in their airways. The mucus makes it easy for bacteria to grow. This leads to repeated, serious lung infections. Over time, these infections can severely damage the lungs.
• Sleep-related breathing disorders that lead to low levels of oxygen in the blood during sleep, such as sleep apnea.
Who needs oxygen therapy?
Oxygen comes in different forms and can be delivered to your lungs in several ways.
Oxygen therapy systems
Oxygen is supplied in three forms: as compressed gas, as liquid, or as a concentrated form taken from the air.
Compressed oxygen gas is stored under pressure in metal cylinders. The cylinders come in various sizes. Some of the cylinders are small enough to carry around with you. You can put them on a small wheeled cart or in a shoulder bag or backpack.
Liquid oxygen is a very cold liquid that becomes gas when released from its container. Liquid oxygen is delivered to your home in a large container. From this container, smaller, more portable units can be filled.
The advantage of liquid oxygen is that the storage units need less space than compressed or concentrated oxygen. However, liquid oxygen costs more than the other forms of oxygen. Also, it evaporates easily, so it doesn't last for a long time.
Oxygen concentrators filter out other gases in the air and store only oxygen. Oxygen concentrators come in several sizes, including portable units.
Oxygen concentrators cost less than the other oxygen therapy systems. One reason is because they don't require oxygen refills. However, oxygen concentrators are powered by electricity. Thus, you'll need a backup supply of oxygen in case of a power outage.
Delivery devices
Most often, oxygen is delivered through a nasal cannula. A nasal cannula consists of two small plastic tubes, or prongs, that are placed in both nostrils.
To help hold the cannula in place, you can put the longer ends of it over your ears or attach them to a special kind of eyeglass frame that helps hide the tubing. The tubing then comes around the back of your ears and under your chin, where it joins together. From there, it's attached to the tube from the oxygen container.
A face mask, which fits over your nose and mouth, may be used instead of a nasal cannula. This method mainly is used if you need a high flow rate of oxygen or if your nose is clogged from a cold.
The face mask may be held in place with a strap that goes around your head or with tubes that fit around your ears. The oxygen is delivered through a tube that attaches to the front of the mask.
Oxygen also may be delivered through a tracheostomy. This is a surgically made hole that goes through the front of your neck and into your windpipe. A breathing tube is placed in the hole to help you breathe. Oxygen delivered this way is called transtracheal oxygen therapy.
If you're on transtracheal oxygen therapy, you'll need to have a humidifier attached to your oxygen system. This is because the oxygen doesn't pass through your nose and/or mouth like it does with the other delivery systems. A humidifier adds moisture to the oxygen and prevents your airways from getting too dry.
Oxygen also can be delivered through breathing machines, such as CPAP (continuous positive airway pressure) devices or ventilators.
Before oxygen therapy
In an emergency – such as a serious accident, possible heart attack, or other life-threatening condition – you may be started on oxygen therapy right away.
Otherwise, your doctor will decide whether you need oxygen therapy based on tests that measure the amount of oxygen in your blood. These tests include an arterial blood gas test and a pulse oximetry test.
For an arterial blood gas test, a small needle is inserted into an artery, usually in your wrist. A sample of blood is taken from the artery. The sample is then sent to a laboratory, where its oxygen level is measured.
For a pulse oximetry test, a small sensor is attached to your fingertip or toe. The sensor uses light to estimate how much oxygen is in your blood.
If the tests show that your blood oxygen level is low, your doctor may prescribe oxygen therapy. In the prescription, your doctor will include the number of liters of oxygen per minute that you need (oxygen flow rate). He or she also will include how often you need to use the oxygen (frequency of use).
Frequency of use includes when and for how long you should use the oxygen. Depending on your condition and blood oxygen level, you may need oxygen only at certain times, such as during sleep or while exercising.
If your doctor prescribes home oxygen therapy, he or she can help you find a home equipment provider to give you with the equipment and other supplies you need.
During oxygen therapy
While you're in the hospital, your doctor will check on you to make sure you're getting the right amount of oxygen. Nurses or respiratory therapists also may assist with the oxygen therapy.
If you're having oxygen therapy at home, a home equipment provider will help you set up the oxygen therapy equipment at your house.
Trained personnel will show you how to use and take care of the equipment. They'll supply the oxygen and teach you how to handle it safely.
Because oxygen poses a fire risk, you'll need to take certain safety steps. Oxygen isn't explosive, but it can worsen a fire. In the presence of oxygen, a small fire can quickly get out of control. Also, the cylinder that compressed oxygen gas comes in can explode when exposed to heat.
Your home equipment provider will give you a complete list of safety steps that you'll need to follow at home and in public. For example, you should:
• Never smoke or be around people who are smoking
• Never use paint thinners, cleaning fluids, gasoline, aerosol sprays, and other flammable materials
• Stay at least 5 feet away from gas stoves, candles, and other heat sources
When you're not using the oxygen, keep it in a large, airy room. Never store compressed oxygen gas cylinders and liquid oxygen containers in small, enclosed places, such as in closets, behind curtains, or under clothes.
Oxygen containers let off small amounts of oxygen. These small amounts can build up to harmful levels if they're allowed to escape into small spaces.
Risks
Oxygen therapy can cause complications and side effects. These problems may include a dry and/or bloody nose, skin irritation from the nasal cannula or face mask, fatigue, and morning headaches.
If these problems persist, tell your doctor and home equipment provider. Depending on the problem, your doctor may need to change your oxygen flow rate or the length of time you're using the oxygen.
If the problem is due to dryness in the nose, your doctor may recommend a nasal spray or have a humidifier added to your oxygen equipment.
If the problem is due to an uncomfortable nasal cannula or face mask, your home equipment provider can help you find a device that fits better. Your provider also can recommend over-the-counter gels and devices that are designed to lessen skin irritation.
Complications from transtracheal oxygen therapy can be more serious. With this type of oxygen therapy, oxygen is delivered through a tracheostomy. This is a surgically made hole that goes through the front of your neck and into your windpipe. A breathing tube is placed in the hole to help you breathe.
Problems that can occur include:
• Mucus balls that develop on the breathing tube inside the windpipe. Mucus balls tend to form as a result of the oxygen drying out the airways. They can cause coughing and clog the windpipe or breathing tube.
• Problems with the breathing tube slipping from the tracheostomy or breaking.
• Infection.
• Injury to the lining of the windpipe.
Proper care and handling of the tracheostomy and related tubes and supplies may reduce the risk of complications.
Other risks
Oxygen poses a fire risk, so you'll need to take certain safety steps. Oxygen itself isn't explosive, but it can worsen a fire. In the presence of oxygen, a small fire can get quickly out of control. Also, the cylinder that compressed oxygen gas comes in can explode when exposed to heat.
Your home equipment provider will give you a complete list of safety steps you'll need to take at home and when out in public.
For example, when you're not using the oxygen, keep it in an airy room. Never store compressed oxygen gas cylinders and liquid oxygen containers in small, enclosed places, such as in closets, behind curtains, or under clothes.
Oxygen containers let off small amounts of oxygen. These small amounts can build up to harmful levels if they're allowed to escape into small spaces.
Living with oxygen therapy
For many people who get oxygen therapy, the supplemental (extra) oxygen allows them to function better and be more active. Oxygen therapy can help in various ways. It may help:
• Decrease shortness of breath and fatigue
• Improve sleep in some people who have sleep-related breathing disorders
• Increase the lifespan of some people who have COPD (chronic obstructive
pulmonary disease)
Although you may need oxygen therapy continuously or for long periods, it doesn't have to limit your daily routine. Portable oxygen units can make it easier for you to move around and do many daily activities. Talk with your doctor if you have questions about whether certain activities are safe for you.
Portable oxygen units also can make it easier for you to travel. Often, the rules for traveling with oxygen vary depending on the transportation carrier (for example, the airline or bus company). If you need oxygen while traveling, plan in advance. Contact your transportation carrier to find out their specific rules.
Also, talk with your doctor and home equipment provider if you're planning to travel. They can help you plan for your oxygen needs and fill out any required medical forms.
Ongoing care
To make sure you're getting the full benefit of your oxygen therapy, visit your doctor regularly. Your doctor can check your progress and adjust your oxygen therapy as needed.
Never change the amount of oxygen you're taking or adjust the flow rate of your oxygen on your own. Discuss any complications or side effects with your doctor first. He or she may recommend adjusting your treatment.
Talk with your doctor about when you should contact him or her or seek emergency medical care. Your doctor can advise you on what to do if you have:
• Increased shortness of breath, wheezing, or other changes from your usual breathing.
• Fever, increased mucus production, or other symptoms of an infection.
• A blue tint to your lips or fingernails. This is a sign that your body isn't getting enough oxygen.
• Confusion, restlessness, or more anxiety than usual.
In an emergency, go to your nearest hospital emergency room or call 911. You may want to consider wearing a medical ID bracelet or necklace to alert others to your medical needs.


