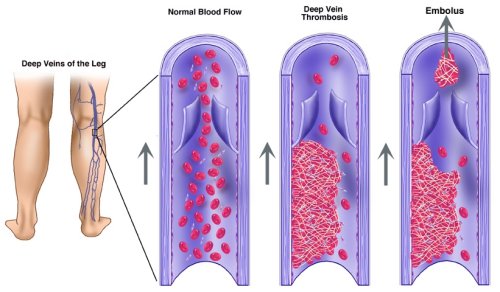
Deep vein thrombosis is a blood clot that forms in a vein deep in the
body. Most deep vein clots occur in the lower leg or thigh. They also can
occur in other parts of the body.
If a clot in a vein breaks off and travels through the bloodstream, it can
lodge in one of the lungs. This is called pulmonary embolism, which is
a very serious condition that can cause death. Blood clots in the thigh
are usually more likely to break off and cause pulmonary embolism than clots
in the lower leg or other parts of the body.
A blood clot also can occur in veins that are close to the surface of the
skin. This type of blood clot is called superficial venous thrombosis or
phlebitis. Blood clots in superficial veins are not dangerous because they
can't travel to the lungs.
Who is
at risk for deep vein thrombosis?
Many factors may increase your risk for deep vein thrombosis:
Having an inherited blood clotting
disorder
Having slowed blood flow – resulting from injury, surgery, or
immobilization – in a deep vein
Having cancer and undergoing treatment
for it
Having other medical conditions, such as varicose
veins
Sitting for a long period of time, for example, on a long trip in
a car or on an airplane
Pregnancy, especially the first 6 weeks after giving birth
Being over age 60 (although deep vein thrombosis can occur in any
age group)
Being overweight
Taking birth control pills or hormone therapy, including for postmenopausal
symptoms
Having a central venous catheter,
which accounts for almost 1 in 10 cases
The risk for deep vein clots increases if a person who has several risk
factors at the same time. For example, a woman with an inherited condition
for clotting who also takes birth control pills has an even higher risk
to have a blood clot.
Signs and symptoms
It is important to see a doctor right away if symptoms of deep vein thrombosis
or pulmonary embolism appear. Deep vein thrombosis can cause very serious
complications if not treated.
Deep vein thrombosis
Only about half of the people with deep vein thrombosis have symptoms. The
symptoms may include:
Swollen area of the leg.
Pain or tenderness in the leg. The pain is usually in one leg and
may be felt only when standing or walking.
Increased warmth in the area of the leg that is swollen or in pain.
Red or discolored skin.
Pulmonary embolism
Some people find out that they have deep vein thrombosis only after the
clot has moved from the leg and traveled to the lung (pulmonary embolism).
The symptoms may include:
Chest pain when taking a deep breath
Shortness of breath
Diagnosis
A doctor will obtain a medical history and carry out an examination in order
to determine if a person has deep vein thrombosis.
Commonly
used tests
Duplex ultrasound is the most commonly used test to diagnose
deep vein clots. It uses sound waves to evaluate the flow of blood in
the veins. A gel is put on the skin of the leg. A handheld device is
placed on the leg and passed back and forth over the affected area.
This device sends sound waves from the leg to an ultrasound machine.
A computer then turns the sound waves into a picture. The picture is
displayed on a TV screen where the doctor can see the blood flow in
the leg. See ultrasound.
Venography may be performed if the duplex ultrasound does not
provide a clear diagnosis. A venogram is an X-ray used to examine veins. A dye, called a contrast
medium, is injected into a vein and then an X-ray is taken of the
leg. The dye makes the vein visible on the X-ray. If the blood flow
in the vein is slowed, it will show on the X-ray.
Less frequently used tests
Magnetic resonance
imaging (MRI) shows pictures of organs and structures inside
the body. MRI uses radio waves to make the image. In many cases, MRI
can provide information that would not show up on an X-ray. This test
is being used more frequently to diagnose deep vein thrombosis.
Computed tomography scan is a special type of X-ray that can provide pictures of structures
inside the body. This test is rarely used to diagnose deep vein thrombosis.
If an inherited blood clotting disorder is suspected, tests may be run for
it. The presence of an inherited clotting disorder is suggested by:
Repeated blood clots that can't be linked to any other cause
Development of a blood clot in a vein at an unusual location, such
as a vein in the liver, kidney, or brain
Treatment
The main goals in treating deep vein thrombosis are to:
Stop the clot from getting bigger
Prevent the clot from breaking off in a vein and moving to the lungs
Reduce the chance of having another blood clot
Medicines
Several types of medicine may be used to treat and/or prevent deep vein
thrombosis:
Anticoagulants decrease
the blood's ability to clot. They are also known as blood thinners.
They are used to stop clots from forming in people who are at risk for
clots and to stop already formed clots from getting bigger. They do
not break up blood clots that have already formed. (The body itself
dissolves most clots over time.)
Anticoagulants can be taken as either a pill (warfarin) or an injection
(heparin).
A doctor may treat a patient with both heparin and warfarin (Coumadin)
at the same time. Heparin acts quickly. Warfarin takes 2 to 3 days before
it starts to work. Once the warfarin starts to work, the heparin is
stopped.
Pregnant women can't take warfarin and are treated with heparin only.
Treatment for deep vein thrombosis with anticoagulants usually lasts
from 3 to 6 months. However, the following situations may change the
length of treatment:
- If the blood clot occurred after a short-term risk (for example,
surgery), the treatment may be shorter.
- In patients who have had clots before, a longer treatment will
be needed.
- In patients who have certain other illnesses, such as cancer,
they may need to take anticoagulants for as long as the illness
is present.
The most common side effect of anticoagulants is bleeding. A doctor
should be informed right away by patients who are taking warfarin or
heparin and have easy bruising or bleeding. Blood
tests can check how well the medicine is working.
Thrombolytics are medicines given to quickly dissolve a blood
clot. They are used to treat large clots that cause severe symptoms.
Because thrombolytics can cause sudden bleeding, they are used only
in life-threatening situations.
Thrombin inhibitors are medicines that interfere with the clotting
process. They are used to treat some types of clots and for patients
who can't take heparin.
Other treatments
Vena cava filters are used when a patient can't take medicines to thin the
blood, or when they are taking blood thinners but continue to develop clots
anyway. The filter is inserted inside a large vein called the vena
cava. The filter catches clots that break off in a vein before they
move through the bloodstream to the lungs (pulmonary embolism). The filter
doesn't prevent new clots from developing. Graduated dvt compression stockings
can reduce the chronic swelling that can occur after a blood clot has developed
in a leg. The leg swelling is due to damage to the valves in the leg veins.
Graduated compression stockings are worn on the legs from the arch of the
foot to just above or below the knee. These
stockings are tight at the ankle and become looser as they go up the leg.
This causes a gentle compression (or pressure) up the leg. The pressure
keeps blood from pooling and clotting.
Some drawbacks of wearing the stockings are:
They can be uncomfortable when worn all day.
They can be hot.
They may be difficult to put on, especially for older adults and overweight
people.
Treatment tips
Much of the treatment for deep vein thrombosis takes place at home. It is
important to:
Take medicines correctly.
Have blood tests done as directed by a doctor.
Avoid activities that may cause serious injury or bleeding.
Talk to a doctor before taking anticoagulants with any other medicines,
especially over-the-counter medicines, at the same time. Over-the-counter aspirin, for example, can thin the blood.
Taking two medicines that thin your blood (even if one is over-the-counter)
may increase the risk for excessive bleeding.
Ask a doctor about dietary factors. Foods that contain vitamin K can
change how well warfarin works. Vitamin K is found in green leafy vegetables
and some oils, such as canola and soybean oil. It is best to eat a well-balanced,
healthy diet that doesn't vary greatly.
Discuss with a doctor what amount of alcohol is safe to drink if also
taking medicine.
Prevention
Preventing deep vein thrombosis depends on whether a person has had a clot
before and on risk factors for developing a clot.
If a deep vein clot has developed before, future clots may be prevented
by:
Taking the medicines prescribed by a doctor to prevent or treat blood
clots
Following up with a doctor for medicine changes and blood tests
In the cases where a person has not had a deep vein clot before but has
risks factors for developing one, it may be possible to prevent a clot by:
Exercising the lower leg muscles, if sitting still for long periods
of time.
Getting out of bed and moving around as soon as possible after a long
period of being bedridden, such as after having surgery or being ill.
The sooner a patient moves around, the less chance they have of developing
a clot.
Taking the medicines prescribed by the doctor to prevent or treat
blood clots after some types of surgery.
Following up with the doctor.