Pancreatic cancer is cancer in which malignant (cancerous) cells
are found in the tissues of the pancreas.
Pancreatic cancer is also called exocrine cancer.
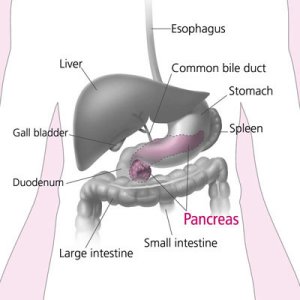
The pancreas
The pancreas is a gland located deep in the abdomen between the stomach and the spine (backbone). The liver, intestine, and other
organs surround the pancreas.
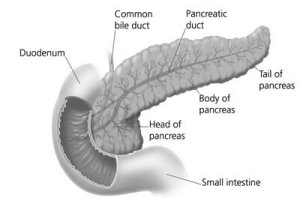
The pancreas is about 6 inches long and is shaped like a flat pear. The
widest part of the pancreas is the head, the middle section is the body,
and the thinnest part is the tail.
The pancreas makes insulin and other hormones.
These hormones enter the bloodstream and travel throughout the body. They
help the body use or store the energy that comes from food. For example,
insulin helps control the amount of sugar in the blood.
The pancreas also makes pancreatic juices. These juices contain enzymes that help digest food. The pancreas releases the juices into a system of
ducts leading to the common bile duct.
The common bile duct empties into the duodenum,
the first section of the small intestine.
Who is at risk?
The exact causes of pancreatic cancer are not known. Doctors can seldom
explain why one person gets pancreatic cancer and another does not.
Research has shown that people with certain risk factors are more likely
than others to develop pancreatic cancer. A risk factor is anything that
increases a person's chance of developing a disease.
Studies have found the following risk factors:
Age. The likelihood of developing pancreatic cancer
increases with age. Most pancreatic cancers occur in people over the
age of 60.
Smoking. Cigarette smokers are two or three times
more likely than nonsmokers to develop pancreatic cancer.
Diabetes. Pancreatic cancer occurs more often in
people who have diabetes than in people who do not.
Being male. More men than women are diagnosed with
pancreatic cancer.
Being African American. African Americans are more
likely than Asians, Hispanics, or whites to get pancreatic cancer.
Family history. The risk for developing pancreatic
cancer triples if a person's mother, father, sister, or brother had
the disease. Also, a family history of colon or ovarian cancer increases
the risk of pancreatic cancer.
Chronic pancreatitis. Chronic pancreatitis is a painful
condition of the pancreas. Some evidence suggests that chronic pancreatitis
may increase the risk of pancreatic cancer.
Other studies suggest that exposure to certain chemicals in the workplace
or a diet high in fat may increase the chance of getting pancreatic cancer.
Most people with known risk factors do not get pancreatic cancer. On the
other hand, many who do get the disease have none of these factors. People
who think they may be at risk for pancreatic cancer should discuss this
concern with their doctor. The doctor may suggest ways to reduce the risk
and can plan an appropriate schedule for checkups.
Signs and symptoms
Pancreatic cancer is sometimes called a "silent disease" because early pancreatic
cancer often does not cause symptoms. But, as the cancer grows, symptoms
may include:
Pain in the upper abdomen or upper back
Yellow skin and eyes, and dark urine from jaundice
Weakness
Loss of appetite
Nausea and vomiting
Weight loss
These symptoms are not sure signs of pancreatic cancer. An infection or
other problem could also cause these symptoms. Only a doctor can diagnose
the cause of a person's symptoms. Anyone with these symptoms should see
a doctor so that the doctor can treat any problem as early as possible.
Diagnosis
If a patient has symptoms that suggest pancreatic cancer, the doctor asks
about the patient's medical history. The doctor may perform a number of
procedures, including one or more of the following:
Physical exam. The doctor examines the skin and eyes
for signs of jaundice. The doctor then feels the abdomen to check for
changes in the area near the pancreas, liver, and gallbladder. The doctor
also checks for ascites, an abnormal buildup of fluid in the abdomen.
Lab tests. The doctor may take blood, urine, and
stool samples to check for bilirubin and other substances. Bilirubin is a substance that passes from the
liver to the gallbladder to the intestine. If the common bile duct is
blocked by a tumor, the bilirubin cannot pass through normally. Blockage
may cause the level of bilirubin in the blood, stool, or urine to become
very high. High bilirubin levels can result from cancer or from noncancerous
conditions.
CT scan (computed tomography). An X-ray machine linked to a computer takes a
series of detailed pictures. The X-ray machine is shaped like a donut
with a large hole. The patient lies on a bed that passes through the
hole. As the bed moves slowly through the hole, the machine takes many
X-rays. The computer puts the X-rays together to create pictures of
the pancreas and other organs and blood vessels in the abdomen.
Ultrasonography. The ultrasound device uses sound
waves that cannot be heard by humans. The sound waves produce a pattern
of echoes as they bounce off internal organs. The echoes create a picture
of the pancreas and other organs inside the abdomen. The echoes from
tumors are different from echoes made by healthy tissues.
The ultrasound procedure may use an external or internal device, or
both types:
- Transabdominal ultrasound. To make images of the pancreas,
the doctor places the ultrasound device on the abdomen and slowly
moves it around.
- EUS (Endoscopic ultrasound). The doctor passes a thin,
lighted tube (endoscope)
through the patient's mouth and stomach, down into the first part
of the small intestine. At the tip of the endoscope is an ultrasound
device. The doctor slowly withdraws the endoscope from the intestine
toward the stomach to make images of the pancreas and surrounding
organs and tissues.
ERCP (endoscopic retrograde cholangiopancreatography).
The doctor passes an endoscope through the patient's mouth and stomach,
down into the first part of the small intestine. The doctor slips a
smaller tube (catheter) through the endoscope into the bile ducts and
pancreatic ducts. After injecting dye through the catheter into the
ducts, the doctor takes X-ray pictures. The X-rays can show whether
the ducts are narrowed or blocked by a tumor or other condition.
PTC (percutaneous transhepatic cholangiography).
A dye is injected through a thin needle inserted through the skin into
the liver. Unless there is a blockage, the dye should move freely through
the bile ducts. The dye makes the bile ducts show up on X-ray pictures.
From the pictures, the doctor can tell whether there is a blockage from
a tumor or other condition.
biopsy. In some cases,
the doctor may remove tissue. A pathologist then uses a microscope to
look for cancer cells in the tissue. The doctor may obtain tissue in
several ways. One way is by inserting a needle into the pancreas to
remove cells. This is called fine-needle aspiration. The doctor uses
X-ray or ultrasound to guide the needle. Sometimes the doctor obtains
a sample of tissue during EUS or ERCP. Another way is to open the abdomen
during an operation.
A person who needs a biopsy may want to ask the doctor the following questions:
What kind of biopsy will I have?
How long will it take? Will I be awake? Will it hurt?
Are there any risks?
How soon will I know the results?
If I do have cancer, who will talk to me about treatment? When?
Staging
When pancreatic cancer is diagnosed, the doctor needs to know the stage,
or extent, of the disease to plan the best treatment. Staging is a careful
attempt to find out the size of the tumor in the pancreas, whether the cancer
has spread, and if so, to what parts of the body.
The doctor may determine the stage of pancreatic cancer at the time of diagnosis,
or the patient may need to have more tests. Such tests may include blood
tests, a CT scan, ultrasonography, laparoscopy,
or angiography. The test results will
help the doctor decide which treatment is appropriate.
Treatment
Read about how pancreatic
cancer is treated.