heart block
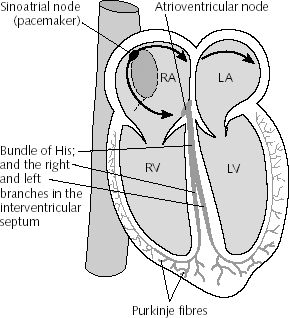
Diagram of heart chambers showing spread of excitation and sites of heart block. (RA, LA: right and left atrium. RV, LV: right and left ventricle.).
Heart block is a problem that occurs with the heart's electrical system. This system controls the rate and rhythm of heartbeats. ("Rate" refers to the number of times the heartbeats in a minute.)
With each heartbeat, an electrical signal spreads across the heart from the upper to the lower chambers. As it travels, the signal causes the heart to contract and pump blood. This process repeats with each new heartbeat.
Heart block occurs when the electrical signal is slowed or disrupted as it moves through the heart.
Overview
Heart block is a type of arrhythmia. An arrhythmia is any problem with the rate or rhythm of the heart.
You can be born with heart block or you can develop it. If you're born with it, it's called congenital heart block. If it develops after birth, it's called acquired heart block.
Acquired heart block is more common. Damage to the heart muscle or to the heart's electrical system causes acquired heart block. Diseases, surgery, or medicines can cause this damage.
Congenital heart block may be found before or after a baby is born. If certain diseases occur during pregnancy, they may cause a baby to be born with heart block. Some congenital heart defects also may cause congenital heart block. Often, doctors don't know what causes these defects.
The three types of heart block are: first degree, second degree, and third degree. First degree is the least severe and third degree is the most severe. This is true for both congenital and acquired heart block.
Doctors use a test called an EKG (electrocardiogram) to help diagnose heart block. This test detects and records the heart's electrical activity. It records the data on a graph so the doctor can review it.
Outlook
The symptoms and severity of heart block depend on which type you have. First-degree heart block rarely causes severe symptoms.
Second-degree heart block may result in the heart skipping a beat or beats. This type of heart block also can make you feel dizzy or faint.
Third-degree heart block limits the heart's ability to pump blood to the rest of the body. This type of heart block may cause fatigue (tiredness), dizziness, and fainting. Third-degree heart block requires prompt treatment, because it can be fatal.
A medical device called a pacemaker is used to treat third-degree heart block and some cases of second-degree heart block. This device uses electrical pulses to make the heart beat at a normal rate.
Types of heart block
First-degree heart block
In first-degree heart block, the electrical signal is slowed as it moves through the heart. When this occurs between the atria and the ventricles, it appears as a slightly longer, flatter line between the P and the R waves on the EKG.
First-degree heart block rarely causes any symptoms. Well-trained athletes and young people are at higher risk for first-degree heart block caused by an overly active vagus nerve. Activity in this nerve slows the heart rate. Some medicines, such as those based on digitalis, also may trigger first-degree heart block.
First-degree heart block usually doesn't require treatment.
Second-degree heart block
In this type of heart block, electrical signals between the atria and ventricles are slowed to a large degree. Some signals can't reach the ventricles. On an EKG, the QRS wave doesn't follow each P wave as it normally would.
If the signal is blocked before it reaches the ventricles, they won't contract and pump blood to the lungs and the rest of the body.
Second-degree heart block is divided into two different types, Mobitz type I and Mobitz type II.
Mobitz type I
In this type (also known as Wenckebach's block), the electrical signals are delayed more and more with each heartbeat, until the heart skips a beat. On the EKG, the delay is shown as a line (called the PR interval) between the P and QRS waves. The line gets longer and longer until the QRS wave doesn't follow the next P wave.
Sometimes people with Mobitz type I feel dizzy or have other symptoms. This type of second-degree heart block is less serious than Mobitz type II.
Mobitz type II
In this type, some of the electrical signals also don't reach the ventricles. However, the pattern is less regular than it is in Mobitz type I. Some signals move between the atria and ventricles normally, while others are blocked. On an EKG, the QRS wave follows the P wave at a normal speed. Sometimes, though, the QRS wave is missing (when a signal is blocked).
Mobitz type II is less common than type I, but it's usually more severe. Some people with type II need medical devices called pacemakers to maintain their heart rates.
Third-degree heart block
In this type of heart block, none of the electrical signals reach the ventricles. This type also is called complete heart block or complete AV block.
When complete heart block occurs, special areas in the ventricles may create electrical signals to cause the ventricles to contract. This natural backup system is slow and isn't coordinated with the contraction of the atria. On an EKG, the normal pattern is disrupted. The P waves occur at a faster rate than the QRS waves.
Complete heart block can be fatal. It can result in sudden cardiac arrest and death. This type of heart block needs emergency treatment. A temporary pacemaker may be used to keep the heart beating until you get a permanent pacemaker.
Causes
Heart block has a number of causes. You can be born with this disorder (congenital) or acquire it.
Congenital heart block
One form of congenital heart block occurs in the babies of women who have autoimmune diseases, such as lupus. People who have these diseases make proteins called antibodies.
In pregnant women, these antibodies can cross the placenta. (The placenta is the organ that attaches the umbilical cord to the mother's womb.) They can damage the baby's heart and lead to congenital heart block.
Congenital heart defects (problems with heart's structure) also may cause congenital heart block. Often, doctors don't know what causes these defects.
Acquired heart block
A number of factors, such as diseases, surgery, medicines, and other conditions, can cause acquired heart block.
The most common cause of acquired heart block is damage to the heart from a heart attack. Other diseases that can cause heart block include coronary artery disease, myocarditis (inflammation of the heart muscle), heart failure, rheumatic fever, and cardiomyopathy.
Other diseases may increase the risk for heart block. These include sarcoidosis and the degenerative muscle disorders, Lev's disease and Lenegre's disease.
Certain types of surgery also may damage the heart's electrical system and lead to heart block.
Exposure to toxic substances and taking certain medicines, including digitalis and beta blockers, also may cause heart block. Doctors closely watch people who are taking these medicines for signs of problems.
In some cases, atrioventricular (AV) heart block has been linked to genetic mutations (changes in the genes).
An overly active vagus nerve can cause first-degree heart block. Activity in this nerve slows the heart rate. Well-trained athletes and young people are at higher risk for first-degree heart block due to this cause.
In some cases, acquired heart block may go away if the factor causing it is treated or resolved. For example, heart block that occurs after a heart attack or surgery may go away after recovery.
Also, if a medicine is causing heart block, the condition may go away if the medicine is stopped or the dosage is lowered. However, you shouldn't change the way you take your medicines unless your doctor tells you to.
Who is at risk
The risk factors for congenital and acquired heart block are different.
Congenital heart block
If a pregnant woman has an autoimmune disease, such as lupus, her fetus is at risk for heart block.
Congenital heart defects also may result in congenital heart block. Most of the time, doctors don't know what causes these defects.
Heredity may play a role in certain heart defects. For example, a parent who has a congenital heart defect may be more likely than other people to have a child with the condition.
Acquired heart block
Acquired heart block can occur in people of any age. However, most types of the disorder are more common in older people. This is because many of the risk factors are more common in older people.
People who have a history of heart disease or heart attacks are more likely to have heart block. Examples of heart disease that can lead to heart block include heart failure, coronary artery disease, and cardiomyopathy.
Other diseases also may raise the risk for heart block. These include sarcoidosis and the degenerative muscle disorders, Lev's disease and Lenegre's disease.
Exposure to toxic substances or taking certain medicines, such as digitalis, can raise your risk for heart block.
Well-trained athletes and young people are at higher risk for first-degree heart block caused by an overly active vagus nerve.
Signs and symptoms
Signs and symptoms depend on the type of heart block you have. First-degree heart block rarely causes symptoms.
Symptoms of second- and third-degree heart block include:
These symptoms may point to other health problems as well. If these symptoms are new or severe, call emergency services or go to the hospital emergency room. If you have milder symptoms, talk to your doctor right away to find out whether you need prompt treatment.
Diagnosis
Heart block may be diagnosed as part of a routine doctor's visit or during an emergency situation (third-degree heart block is an emergency).
Your doctor will diagnose heart block based on your family and medical histories, a physical exam, and results from tests.
Specialists involved
Your primary care doctor may be involved in diagnosing heart block. However, if you have the condition, you may need to see a heart specialist. Heart specialists include:
Family and medical histories
To find out your family and medical histories, your doctor may ask whether:
Your doctor also may ask about other health habits, such as how much physical activity you do.
Physical exam
During the physical exam, your doctor will listen to your heart's rhythm. He or she will listen carefully for abnormal rhythms or heart murmurs (extra or unusual sounds heard during heartbeats).
Your doctor also may:
Diagnostic tests and procedures
EKG (electrocardiogram)
Doctors usually use a test called an EKG (electrocardiogram) to help diagnose heart block. This simple test detects and records the heart's electrical activity. It shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
The data is recorded on a graph. Different types of heart block have different patterns on the graph.
A standard EKG test only records the heart's activity for a few seconds.
Holter and event monitors
To diagnose first- or second-degree heart block, your doctor may have you wear a Holter monitor or an event monitor.
Holter and event monitors are similar to EKGs, but they're portable devices. You can wear a Holter or event monitor while you do your normal daily activities. This allows the device to record your heart's electrical activity for a longer time than an EKG.
Electrophysiology study
For some cases of heart block, doctors may do electrophysiology studies (EPS). During an EPS, a thin, flexible wire is passed through a vein in your groin (upper thigh) or arm to your heart. The wire records your heart's electrical signals.
Other tests
To diagnose heart block, your doctor may need to do tests to rule out other types of arrhythmias (irregular heartbeats).
Treatment
Treatment depends on the type of heart block you have. First-degree heart block usually needs no treatment.
If you have second-degree heart block, you may need a pacemaker. A pacemaker is a small device that's placed under the skin of the chest or abdomen. This device uses electrical pulses to stimulate the heart to beat at a normal rate.
If you have third-degree heart block, you will need a pacemaker. In an emergency, a temporary pacemaker may be used until you can get a permanent one. Most people who have third-degree heart block need pacemakers for the rest of their lives.
Some people with third-degree congenital heart block don't need a pacemaker for many years. Others may need a pacemaker at a young age or during infancy.
In some cases, acquired heart block may go away if the factor causing it is treated or resolved. For example, heart block that occurs after a heart attack or surgery may go away.
Also, if a medicine is causing heart block, the condition may go away if the medicine is stopped or the dosage is lowered. However, you shouldn't change the way you take your medicines unless your doctor tells you to.
Living with heart block
First-degree heart block may not cause any symptoms or require treatment. If you've been diagnosed with this condition, ask your doctor whether you need to take any special measures to control it. Your doctor can tell you whether you need ongoing care or whether you need to change the way you take certain medicines.
If you have second-degree heart block that doesn't require a pacemaker, talk to your doctor about keeping your heart healthy. Your doctor will tell you whether you need ongoing care for your condition.
Living with a pacemaker
People who have third-degree heart block and some people who have second-degree heart block need pacemakers. If you have a pacemaker, you should take special care to avoid things that may interfere with it.
Avoid close or prolonged contact with electrical devices and devices that have strong magnetic fields. These objects can keep your pacemaker from working properly.
Let all of your doctors, dentists, and medical technicians know that you have a pacemaker. You also should notify airport screeners.
Certain medical procedures can disrupt pacemakers. These include MRI (magnetic resonance imaging), electrocauterization during surgery, and shock-wave lithotripsy to get rid of kidney stones.
Your doctor may need to check your pacemaker several times a year to make sure it's working properly. Some pacemakers must be checked in the doctor's office, but others can be checked over the phone.
Ask your doctor about what types of physical activity are safe for you. A pacemaker usually won't limit you from doing sports and physical activity. But you may need to avoid full-contact sports, such as football, that can damage the pacemaker.


