AIDS and HIV
Figure 1. HIV budding from an infected cell. Image source: NIAID.

Figure 2. HIV virion. Image source: NIAID.
Figure 3. HIV replication cycle. Image source: NIAID.

Figure 4. Scanning electron micrograph of HIV-1, colored green, budding from a cultured lymphocyte.Image source: CDC.
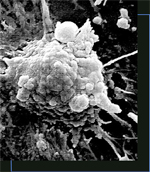
Figure 5. An HIV-infected cell undergoing apoptosis. Image source: Institute of Cell and Molecular Science.
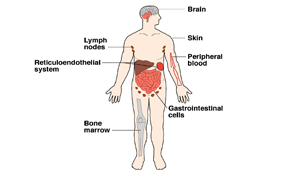
Figure 6. HIV can hide in the brain, lymph nodes, skin, peripheral blood, reticuloendothelial system, bone marrow, and gastrointestinal cells.
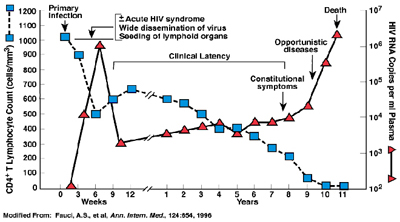
Figure 7. Typical course of HIV infection that shows the relationship between the levels of HIV (viral load) and CD4+ T cell counts over the average course of untreated HIV infection.
AIDS is a disease caused by a retrovirus, called human immunodeficiency virus (HIV), that mainly attacks T-4 cells (which help the production of antibodies) and renders the body's immune system incapable of resisting infection (Figures 1 and 2). The first diagnosis was in New York in 1979. In 1983–1984 scientists at the Pasteur Institute in France and the National Cancer Institute in the USA isolated HIV as the cause of the disease.
The virus can remain dormant in infected T-cells for up to 10 years. Early symptoms include severe weight loss and fatigue. The condition progresses to full-blown AIDS, characterized by secondary infections, neurological damage, and cancers (such as Kaposi's sarcomas and B-cell lymphomas).
AIDS is transmitted only by a direct exchange of body fluids. Methods of transmission include: sexual intercourse, sharing of contaminated needles by intravenous drug users, and infected mothers to their babies in the uterus. Before effective screening procedures were introduced many hemophiliacs were infected through transfusions of contaminated blood. Development of a vaccine has been hampered by the virus' constantly shifting genetic composition. Research has centered on treatment, and on delaying the onset of the full-blown syndrome. In 1986–1987 the first chemical was produced which was partially successful in controlling symptoms, zidovudine or azidothymidine (AZT). More recently the emphasis has been on reducing the viral load – the amount of virus within the body – using a combination of AZT and newer drugs such as protease inhibitors.
How HIV causes AIDS
HIV destroys CD4 positive (CD4+) T cells, which are white blood cells crucial to maintaining the function of the human immune system. As HIV attacks these cells, the person infected with the virus is less equipped to fight off infection and disease, ultimately resulting in the development of AIDS.
 |
| Normal T-cells. Image source: NIAID. |
 |
| HIV-infected T-cells. Image source: NIAID. |
Most people who are infected with HIV can carry the virus for years before developing any serious symptoms. But over time, HIV levels increase in the blood while the number of CD4+ T cells decline. Antiretroviral medicines can help reduce the amount of virus in the body, preserve CD4+ T cells and dramatically slow the destruction of the immune system.
People who are not infected with HIV and generally are in good health have roughly 800 to 1,200 CD4+ T cells per mm3 of blood. Some people who have been diagnosed with AIDS have fewer than 50 CD4+ T cells in their entire body.
Biology of HIV
HIV belongs to a class of viruses known as retroviruses. Retroviruses are viruses that contain RNA (ribonucleic acid) as their genetic material. After infecting a cell, HIV uses an enzyme called reverse transcriptase to convert its RNA into DNA (deoxyribonucleic acid) and then proceeds to replicate itself using the cell's machinery.
Within the retrovirus family, HIV belongs to a subgroup known as lentiviruses, or "slow" viruses. Lentiviruses are known for having a long time period between initial infection and the beginning of serious symptoms. This is why there are many people who are unaware of their HIV infection, and unfortunately, can spread the virus to others.
Similar versions of HIV infect other nonhuman species, such as feline immunodeficiency virus (FIV) in cats and simian immunodeficiency virus (SIV) in monkeys and other nonhuman primates. Like HIV in humans, these animal viruses primarily infect immune system cells, often causing immune deficiency and AIDS-like symptoms. These viruses and their hosts have provided researchers with useful, although imperfect, models of the HIV disease process in people.
Structure of HIV
the viral envelope
HIV is spherical in shape and has a diameter of 1/10,000 of a millimeter. The outer coat of the virus, known as the viral envelope, is composed of two layers of fatty molecules called lipids, taken from the membrane of a human cell when a newly formed virus particle buds from the cell. Embedded throughout the viral envelope are proteins from the host cell, as well as 72 copies (on average) of a complex HIV protein known as Env. These Env copies protrude or spike through the surface of the virus particle (called a "virion"). Env consists of a cap made of three molecules called glycoprotein 120 (gp120), and a stem consisting of three molecules called gyclycoprotein 41 (gp41) that anchor the structure in the viral envelope. Much of the research to develop a vaccine to prevent HIV infection has focused on these envelope proteins.
the viral core
Within the viral envelope is a bullet-shaped core or capsid, made up of 2,000 copies of the viral protein, p24. The capsid surrounds two single strands of HIV RNA, each of which has a complete copy of the virus's genes. HIV has three structural genes (gag, pol, and env) that contain information needed to make structural proteins for new virus particles. The env gene, for example, codes for a protein called gp160 that is broken down by a viral enzyme to form gp120 and gp41, the components of the env protein.
HIV has six regulatory genes (tat, rev, nef, vif, vpr, and vpu) that contain information needed to produce proteins that control the ability of HIV to infect a cell, produce new copies of virus, or cause disease. The protein encoded by nef, for instance, apparently is necessary for the virus to replicate efficiently, and the vpu-encoded protein influences the release of new virus particles from infected cells. Recently, researchers discovered that vif (the protein encoded by the vif gene) interacts with an antiviral defense protein in host cells (APOBEC3G), causing inactivation of the antiviral effect and enhancing HIV replication. This interaction may serve as a new target for antiviral drugs.
The ends of each strand of HIV RNA contain an RNA sequence called the long terminal repeat (LTR). Regions in the LTR act as switches to control production of new viruses and can be triggered by proteins from either HIV or the host cell.
HIV's core also includes a protein called p7, the HIV nucleocapsid protein. Three enzymes carry out later steps in the virus's life cycle: reverse transcriptase, integrase, and protease. Another HIV protein called p17, or the HIV matrix protein, lies between the viral core and the viral envelope.
HIV replication cycle
Steps in the HIV replication cycle
See Figure 5. The steps are as follows:
HIV replication cycle glossary
CD4 – a large glycoprotein that is found on
the surface of helper T cells, regulatory T cells, monocytes, and dendritic
cells. Its natural function is as a coreceptor that assists the T cell
receptor (TCR) to activate its T cell following an interaction with an antigen
presenting cell. CD4 is a primary receptor used by HIV–1 to gain entry into
host T cells.
Coreceptor (CCR5 or CXCR4) – protein molecules
on the surface of lymphocytes or monocytes that bind to the gp120 protein
of HIV and facilitate, usually with CD4, entry of viral nucleic acid and
proteins into the cell.
DNA (deoxyribonucleic acid) – is a nucleic
acid that contains the molecular basis of heredity for all known living
organisms and some viruses and is found in the nuclei and mitochondria of
eukaryotes. Chemically DNA consists of two polymer strands of units called
nucleotides made up of one of four possible bases plus sugar and phosphate
groups. The polymers are joined at the bases by hydrogen bonds to form a
double helix structure.
Fusion of virus and cell membranes – a merging
of cell and virus membranes that permits HIV proteins and nucleic acids
to enter the host cell.
Genomic RNA – the nucleic acid that contains
all of the hereditary information of a virus, and is found in a mature virion.
gp120 – an HIV glycoprotein having a molecular
weight of 120 that protrudes from the outer surface of the virion. This
glycoprotein binds to a CD4 receptor on a T cell to facilitate entry of
viral nucleic acid and proteins into the cell.
HIV (human immunodeficiency virus) – is a lentivirus
and a member of the retrovirus family. HIV infects and destroys helper T
cells of the immune system causing a marked reduction in their numbers.
Loss of CD4 cells leads to generalized failure of the immune system and
susceptibility to life threatening opportunistic infections.
Integrase – An enzyme found in retroviruses
including HIV that permits the viral DNA to be integrated into the DNA of
the infected cell.
Preintegration complex (PIC) – It is composed
of viral RNA and proteins (nucleocapsid, p6, Vpr, integrase, and matrix)
as well as some host proteins. It functions to reverse transcribe genomic
RNA into double stranded DNA prior to integration into the host genomic
DNA.
Protease – an enzyme that hydrolyzes or cuts
proteins and is important in the final steps of HIV maturation.
Nucleus – a membrane enclosed cellular organelle
of eukaryotes that functions to contain the genomic DNA and to regulate
gene expression.
Reverse transcriptase – an enzyme found in
HIV that creates double stranded DNA using viral RNA as a template and host
tRNA as primers.
RNA (ribonucleic acid) – a nucleic acid that
differs from DNA in that it contains ribose and uracil as structural components.
RNA virus – a virus that uses RNA as its genetic
material and belongs to either Group III, IV, or V of the Baltimore Classification
System of Viruses. HIV belongs to Group III, double stranded RNA viruses.
Virion – a single and complete extracellular
infective form of a virus that consists of an RNA or DNA core with a protein
coat or "envelope".
HIV evolves to evade the immune system
HIV replicates rapidly with several billion new viruses made every day in a person infected with HIV. What makes HIV so difficult to stop, however, is its ability to mutate and evolve.
Reverse transcriptase, the enzyme that makes DNA copies of HIV's RNA, often makes random mistakes. As a result, new types or strains of HIV develop in a person infected with HIV. Some strains are harder to kill because of their ability to infect and kill other types of cells, while other strains replicate at faster rates. The more virulent and infectious strains of HIV are typically found in people who are in the late stages of infection. Different strains of HIV can also recombine to produce an even wider range of strains. In essence, HIV is constantly changing and trying to evade the immune system. Its ability to evolve rapidly is one of the major reasons why HIV is such a deadly virus.
HIV devastates the immune system
Every day, HIV destroys billions of CD4+ T cells in a person infected with HIV, eventually overwhelming the immune system's capacity to regenerate or fight other infections. The following are different ways this may occur:
Killing cells directly
CD4+ T cells infected with HIV may be killed when a large amount of virus is produced and buds out from the cell surface. The budding process disrupts the cell membrane and causes the cell to die. The cell can also expire when the virus excessively uses the cell's machinery for its own purposes, disrupting normal activities needed for the survival of the cell.
Apoptosis (cell suicide)
When the regulation of a cell's machinery and functions become grossly distorted because of HIV replication, the infected cell may commit suicide by a process known as programmed cell death or apoptosis. There is evidence that apoptosis occurs most frequently in the bloodstream and lymph nodes of people infected with HIV.
The death of innocent bystander cells
Cells that are not infected with HIV may also die as a direct result of the effects of HIV infection:
Destruction of immune precursor cells
Studies suggest that HIV also destroys precursor cells (young cells that have not yet fully developed) that later mature into cells with special immune functions. HIV can also damage the bone marrow and the thymus, which are needed for developing precursor cells. The bone marrow and thymus probably lose their ability to regenerate, further compounding the suppression of the immune system.
HIV hides from the immune system
When HIV infects a cell, the virus can hide within the cytoplasm (the jelly-like fluid that fills the cell) or integrate into the cell's genetic material (chromosomes). Shielded from the immune system, HIV can lie dormant in an infected cell for months or even years. These cells serve as a latent reservoir of the virus.
Antiretroviral drugs are capable of suppressing HIV, even to undetectable levels in the blood, but they cannot eliminate the virus hiding in these latent reservoirs. A key research priority is to learn how HIV establishes these latent reservoirs and to develop strategies to purge the virus from the body.
Clinical progression of HIV
Acute primary infection
Once HIV enters the body, the virus infects a large number of CD4+ T cells and replicates rapidly. During this acute phase of infection, the blood has a high number of HIV copies (viral load) that spread throughout the body, seeding in various organs, particularly the lymphoid organs such as the thymus, spleen, and lymph nodes. During this phase, the virus may integrate and hide in the cell's genetic material. Shielded from the immune system, the virus lies dormant for an extended period of time. In the acute phase of infection, up to 70% of HIV-infected people suffer flu-like symptoms.
The immune system strikes back
Two to four weeks after exposure to the virus, the immune system fights back with killer T cells (CD8+ T cells) and B-cell-produced antibodies. At this point, HIV levels in the blood are dramatically reduced. At the same time, CD4+ T cell counts rebound and for some individuals, the number rises to its original level.
Clinical latency
During this phase, a person infected with HIV may remain free of HIV-related symptoms for several years despite the fact that HIV continues to replicate in the lymphoid organs where it initially seeded.
Progression to AIDS
The immune system eventually deteriorates to the point that the human body is unable to fight off other infections. The HIV viral load in the blood dramatically increases while the number of CD4+ T cells drops to dangerously low levels. An HIV-infected person is diagnosed with AIDS when he or she has one or more opportunistic infections, such as pneumonia or tuberculosis, and has fewer than 200 CD4+ T cells per cubic millimeter of blood.
Factors that affect HIV progression
Mutations in HIV co-receptors
Most strains of HIV use a co-receptor molecule called CCR5, in addition to the CD4 molecule, to infect a cell. Other HIV strains use a different co-receptor known as CXCR4 to attack cells. Both receptors enable the virus to enter a cell during the initial stage of HIV infection.
Studies have shown that people infected with HIV who have specific genetic mutations in one of their two copies of the CCR5 gene progress to AIDS slower than people with two normal copies of the CCR5 gene. There are also rare individuals with two mutant copies of the CCR5 gene who appear, in most cases, to be completely protected from HIV infection. Gene mutations in other HIV co-receptors such as CXCR4 also may influence the rate of disease progression.
High viral load
The amount of HIV in a person's blood often is called his or her viral load. People with high viral loads are more likely to progress to AIDS faster than people with lower levels of the virus. In addition, research has shown that the level of HIV in a person's blood after the first few months of infection, known as the viral set point, also influences the speed of progression to AIDS. Those with higher viral set point are much more likely to get sick faster than those with lower viral set point.
Highly active antiretroviral therapy (HAART), which is a potent combination of three or more antiretroviral drugs belonging to at least two different antiretroviral drug classes, can help lower the viral load and viral set point for those infected with HIV. For many people, HAART delays the progression to AIDS for a prolonged period of time.
HIV risk factors
HIV is found in the blood, semen, or vaginal fluid of someone who is infected with the virus. You may be at increased risk of becoming infected with HIV if you:
Quick facts about HIV transmission
Symptoms
Early symptoms
In the initial stages of HIV infection, most people will have very few, if any, symptoms. Within a month or two after infection, individuals may experience a flu-like illness, including:
These symptoms usually disappear within a week to a month and are often mistaken for another viral infection, such as influenza (flu). However, during this period people are highly infectious because HIV is present in large quantities in genital fluids and blood. Some people infected with HIV may experience more severe symptoms initially or a longer duration of clinical symptoms, while others may remain symptom-free for 10 years or more.
Later symptoms
During the late stages of HIV infection, the virus severely weakens the immune system, and people infected with the virus may experience the following symptoms:
Each of these symptoms can be related to other illnesses. The only way to determine if you are infected with HIV is to get tested.
Testing and diagnosis
Routine HIV testing
Of the estimated 1.1 million Americans currently living with HIV, 21% do not know they are infected. People who have been recently infected with HIV often have few to no symptoms yet are extremely infectious and, therefore, may unknowingly transmit the virus to others. Therefore, the US Centers for Disease Control and Prevention (CDC) recommends HIV testing for adults, adolescents, and pregnant women during routine medical care.1 Regular HIV screenings allow healthcare providers to identify people who are not aware that they are infected with HIV, so that they can be counseled on the need to avoid high-risk behaviors, instructed on safe-sex practices and given information about starting antiretroviral therapy. HIV testing can also be performed anonymously if a person is concerned about confidentiality.
Types of HIV tests
Healthcare providers can test a sample of blood to see if it contains human antibodies (disease-fighting proteins) specific to HIV. The two key types of HIV antibody tests are the enzyme-linked immunosorbent assay (ELISA) and the Western blot.
However, these antibody tests may not detect HIV antibodies in someone who has been recently infected with HIV (within one to three months of infection). In these situations, healthcare providers can test the blood for the presence of HIV genetic material. This test is extremely critical for identifying recently infected individuals who are at risk for unknowingly infecting others with HIV.
HIV testing in infants
The CDC recommends that all pregnant women get tested for HIV before and/or during delivery. Knowing the HIV status of the mother allows physicians to prevent mother-to-child HIV transmission by providing antiretroviral treatment to both mothers infected with HIV and their newborn infants. However, it is difficult to determine if a baby born to a mother infected with HIV is actually infected because babies carry their mothers' HIV antibodies for several months. Today, healthcare providers can conduct an HIV test for infants between ages 3 mo and 15 mo. Researchers are now evaluating several blood tests to determine which ones are suitable for testing babies younger than 3 mo.
Treatment of HIV infection
In the early 1980s when the HIV/AIDS epidemic began, people with AIDS were not likely to live longer than a few years. Today, there are 31 antiretroviral drugs (ARVs) approved by the US Food and Drug Administration (FDA) to treat HIV infection. These treatments do not cure people of HIV or AIDS. Rather, they suppress the virus, even to undetectable levels, but they do not completely eliminate HIV from the body. By suppressing the amount of virus in the body, people infected with HIV can now lead longer and healthier lives. However, they can still transmit the virus and must continuously take antiretroviral drugs in order to maintain their health quality.
Prevention
Currently, there is no vaccine to prevent HIV infection nor is there a cure for HIV/AIDS. To reduce your risk of becoming infected with HIV or transmitting the virus to others:


