fractures and dislocations
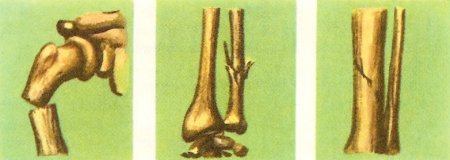
Figure 1. Types of fracture, I. From left to right: fractured humerus with displacement; fracture of the ulna, in the forearm; incomplete fracture of the tibia.
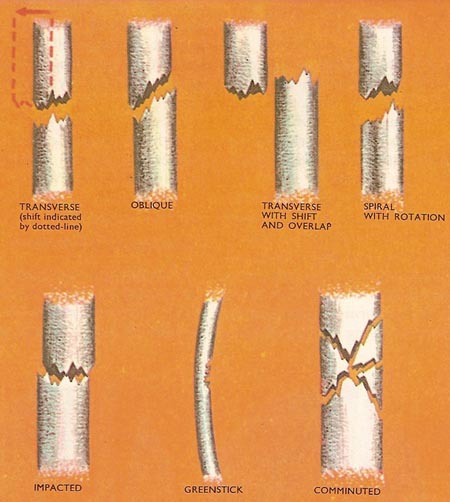
Figure 2. Types of fracture, II. See text for details.
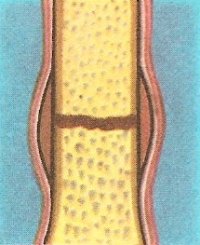
Figure 3. Stages of healing after a fracture: 1. Considerable bleeding occurs at the fracture. The blood lies between the bone ends and under the periosteum.
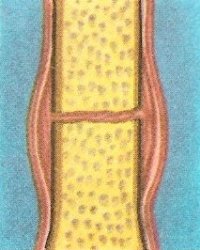
Figure 4. Stages of healing: 2. In a few days a blood clot forms. Soon the clot is invaded by osteoblasts from the nearby bone and from the periosteum.
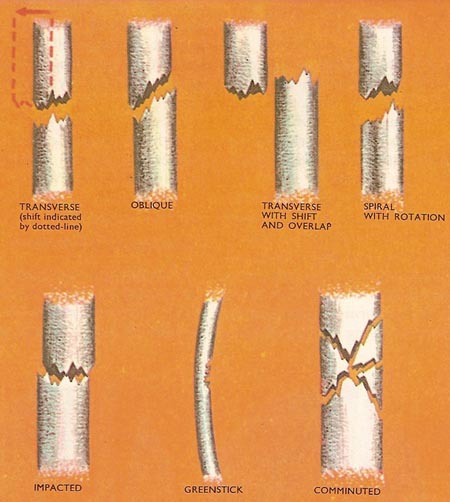
Figure 5. Stages of healing: 3. The osteoblasts lay down new bone which fills the gap between the fragments and bulges out at the sides. This is the callus.
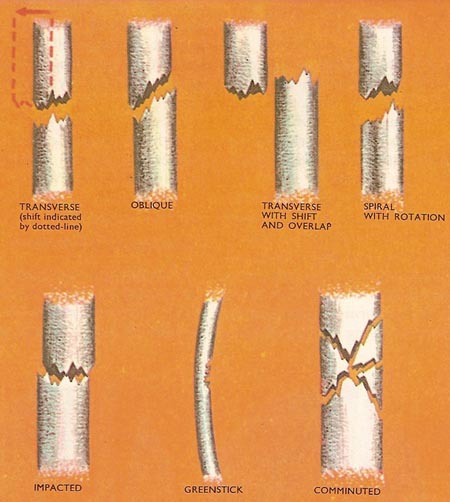
Figure 6. Stages of healing: 4. Over a period of many months the callus is absorbed by the osteoblasts, and they make more new bone exactly like the original one.
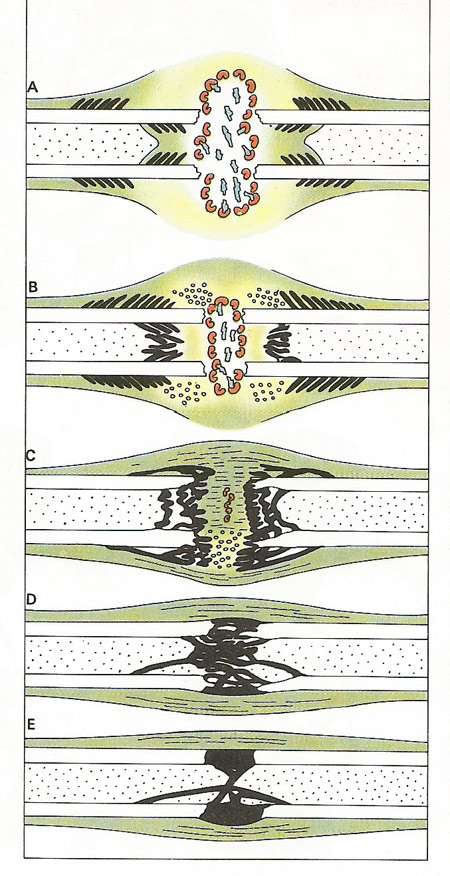
Figure 7. After a fracture inflammation sets in and a blood clot forms, sealing the ends of damaged vessels (A). Macrophages invade the site, and remove the wound debris; then after one or two days, long, thin fibroblasts lay down a mesh or grid on which new tissue can grow (B). A blastema or area of new growth develops and new bone is forged that links the broken ends (C). Later remodeling strengthens the bone, restoring its true shape (D, E). At least four to six weeks are required for a fracture to heal completely.
Although is bone is very hard and strong, even the largest and thickest bones in the body are sometimes broken, or moved out of place at the joint. This can happen if a bone is knocked violently or if it is forcibly bent or twisted.
The medical term for a break in a bone is a fracture. If a bone is not in its correct location but is not broken, it is said to be dislocated.
Types of fracture
In a simple, or closed, fracture the skin over the injured bone is unbroken and there is no communication between the fracture and the outside of the body. A compound, or open, fracture is one in which the skin over the break is torn, or lacerated, and parts of the broken bone may even show through. When the fragments move out of their correct positions, after a bone is broken, there is said to be displacement. Because in a compound fracture there is an external wound leading to the site of the fracture, this type of injury is liable to infection by disease-causing bacteria, a fact which may have an important bearing on the treatment. There is no risk of infection with a simple fracture. (Figure 1.)
The pattern of fracture is a clue to the cause of the break and often indicates the best way to draw the broken ends of the bone together, a process called reduction. A transverse fracture is one across the bone approximately at right angles to its length. Oblique fractures are diagonal to the length of the bone, and spiral fractures are irregular diagonal breaks caused by the sharp twisting of a bone. (Figure 2.)
Comminuted fractures are those in which the bone is broken into more than two pieces. In an impacted fracture one of more fragments of bone is driven into another and they become interlocked. Compression fractures are caused by crushing of bone; greenstick fractures occur only in the flexible bones of young children and are incomplete breaks: they may be compared with the breaks produced on the concave side of a green sapling by bending it like an archer's bow.
The term depressed fracture is only used for the skull when a bone is driven inwards.
Causes of fractures
The various types of fracture may result from three main causes: (1) sudden injury, (2) fatigue, (3) disease. Fractures of the first type are by far the most common and are sudden breaks in healthy bones as the result of an applied force. A bone may break from a direct blow, as may happen to the tibia (shinbone) in a heavy tackle while playing soccer – or it may break from an indirect blow. For example, the head of the radius (a bone in the forearm) is often fractured as a result of a fall onto an outstretched hand.
Fatigue or stress fractures are due to the repeated application of stress. Generally they affect only the bones of the legs, especially the foot, though the neck of the femur (thigh bone) and the bones immediately below the knee (tibia and fibula) may also break.
Disease or pathological fractures may result from a number of unhealthy conditions. The bones are so weakened that they may break through the slightest force being applied to them. Even the weight of the body carried in walking may be sufficient in extreme cases.
Symptoms
Pain is the most obvious symptom of a fracture. It begins at the moment of injury and may be very severe.
Because of the pain, and because the framework of the injured part is broken, it is often impossible to move the damaged part.
The tissues all round the fracture swell up, and where there is displacement of the fragments of a broken bone the injured part may have an unnatural shape.
Diagnosis and treatment
A suspected fracture should always be examined by a doctor, who may order an X-ray to see how much damage has been done.
Simple fractures without displacement generally heal quickly if they are kept still in plaster of Paris. Compound fractures and fractures with displacement need surgical treatment before the plaster is put on.
The first stage in the treatment of a fracture is called reduction. This involves placing the bone ends together so that they are in contact with one another. They will only unite if in contact. The whole operation is carried out carefully to ensure that the placing of the repositioned bones is accurate.
In some cases reduction of a fracture should not be attempted, as in a grooved fracture of the skull, but in most cases it is necessary. It should then be attempted without delay before the hematoma clots (see below) or before callus formation takes place. The patient is anesthetized so that the reduction is painless and the risk of a muscle contracting and displacing the broken parts is eliminated. The method of reduction depends on the nature of the fracture. For example, if one half of the bone overlaps the other (it usually shifts to one side as well) the bone is pulled, the shift is corrected, and the bone is then released so that the ends come into contact. Alternatively the fragments are angled so that they lie parallel and the ends are then turned and brought into contact in the correct position.
When fragments of bone cannot be manipulated easily, an open operation is necessary. Special instruments, used in a similar way to a shoehorn, are used to reposition the exposed fragments.
Depending on where the fracture occurs and how serious it is, one of two kinds of splint may be used. External splints are applied outside (e.g., plaster-of-Paris) while internal splints actually lie within the tissues.
A familiar method of splinting uses plaster-of-Paris strips. The strips are applied when wet and evenly molded to the limb by binding them on tightly.
Plaster bandages may also be wound round and round. It is usual to use a layer of muslin inside the plaster to prevent it from sticking to the hairs, thus easing its removal at a later date.
In some fractures (e.g., fractures of the femur shaft) some other support is needed besides a plaster splint in order to hold the bone fragments in the correct position. One method is to balance the pull of the muscles by a weight (this is known as traction). The pull of the weight is continuous. Usually some other support is given to the limb as well.
Methods of fixing fractures internally include using pins inside the hollow core of the bone, screws, a metal plate held in place by screws, or a bone graft, acting as a plate, and screws. Internal fixation is used when methods of splinting or splinting combined with traction are inadequate.
Healing of a fracture
In bone, the cells are arranged in small groups within the substance of the bone and also under the periosteum, a tightly fitting membrane which covers the surface of each bone. They are called osteoblasts, which means "bone-forming cells." Their task is to collect the calcium from the blood and to deposit it around themselves in the form of calcium phosphate and calcium carbonate, which are salts that are insoluble in water. It is the mixture of these two salts which provides bone with its remarkable hardness and rigidity.
Following a fracture, blood seeps out of torn blood vessels and the gap between the fracture surfaces is filled up. The fluid is prevented from escaping by muscle tissue and the torn outer covering or periosteum of the bone. The blood clots to a jelly-like consistency so that the fracture is surrounded by, and filled with, a gluey mass. This is called a hematoma (Figure 3).
Slowly, the hematoma becomes organized. It is penetrated by fine capillaries that formed a much branched network within (Figure 4). Gradually the tissue becomes firmer due to the deposition of calcium until it forms a rigid bond across the fracture. This calcified callus, as it is called, is invaded by bone cells. These absorb the calcium in the callus and replace it by bone (Figure 5).
X-rays at this stage show that the gap between the ends is filled with bone and the whole repair is surrounded by surplus callus. The new bone has yet to obtain its usual layered structure. Gradually it is reorganized, at the expense of unwanted callus, to take up the stresses that the bone has to bear (Figure 6).
In children the remodeling is eventually so complete that usually no trace of the fracture can be seen in X-ray photographs. Healing is never so complete in the adult and some thickening at the site of fracture is inevitable. In young children complete healing may be obtained in about six weeks but in adults it takes a minimum period of four to five months for a bone such as the femur to mend.
When disease has weakened a bone, and it is fractured, repair may not always follow, though radiation treatment or the use of hormones increases the chance of a repair ensuing in certain conditions (e.g., when a fracture occurs through the region of a bone tumor). In most diseases where there is an abnormality in bone formation there is usually slow healing of fractures (e.g., rickets).
History of treatment of fractures
Although records of the treatment of fractures date back at least to ancient Egyptian times, their precise treatment has only been possible since the beginning of the 20th century. From this time great advances in fracture surgery were made, due largely to the discovery of X-rays by Wilhelm Röntgen in 1895. He noted, while experimenting with a cathode ray tube, that the pattern of the bones of his hand was visible on a fluorescent screen when it was held between the tube and the screen. From this early apparatus a vast range of modern X-ray equipment has evolved. Until the advent of X-ray imaging, surgeons worked in the dark, setting fractures by touch alone.
The introduction of antiseptics into surgery in the second half of the 19th century by Lister, and the subsequent introduction of antibiotics, permitted more difficult operations to be carried out, particularly those involving compound fractures. Prior to Lister's time open operations were virtually not allowed because of the great risk of infection.
Even with aseptic surgery and the use of X-rays to determine the true extent of a fracture, many problems remained to be solved and, of course, many advances are still being made. One problem that remained for many years was that of finding a suitable metal with which to "pin" together shattered pieces of bone. Iron, mild steel, and silver corrode away inside the tissues and the resulting chemical changes often slow down the healing of the fractured bone. Eventually the development of special alloys solved this problem.
Great progress was made in other directions, too. It was realized that in many cases the part containing the fractured bone need not be kept completely still while the fracture was mending. Muscles quickly waste away if they are not used for some time. Special exercises were devised so that this was avoided. The physiotherapist gained an important role in this respect.
Dislocations
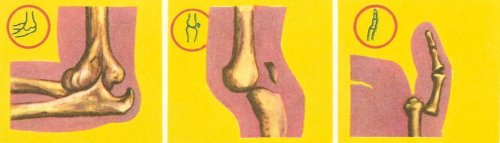
When a joint, instead of a bone, suffers a severe strain, the result may be a dislocation. In an injury of this kind no bones are broken, but one bone is pushed out of its proper place (Figure 8).
Dislocated joints are very painful. They usually look deformed because the bones are in the wrong position.
Illustrated here are three quite common dislocations. The drawings in the red circles show how the bones should normally look.
The process of putting the bones back into their normal positions in a joint is called reduction of the dislocation. The patient is typically given an anesthetic which relaxes his or her muscles. The surgeon can then usually get the bones back into their proper positions quite readily.
When a joint is dislocated there is bound to be some stretching of the parts round it. This can mean that the joint is loosened and later may be dislocated again.


