thyroid cancer
Thyroid cancer is cancer that forms in the thyroid gland (an organ at the base of the throat that makes hormones that help control heart rate, blood pressure, body temperature, and weight). The four main types of thyroid cancer are papillary, follicular, medullary, and anaplastic thyroid cancer. These four types are based on how the cancer cells look under a microscope.
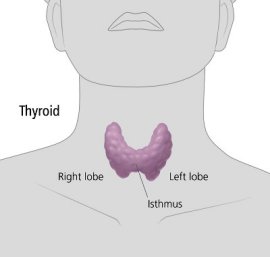
Thyroid gland
The thyroid is a gland in the neck. It has two kinds of cells that make hormones. Follicular cells make thyroid hormone, which affects heart rate, body temperature, and energy level. C cells make calcitonin, a hormone that helps control the level of calcium in the blood.
The thyroid is shaped like a butterfly and lies at the front of the neck, beneath the larynx (voice box). It has two parts, or lobes. The two lobes are separated by a thin section called the isthmus.
A healthy thyroid is a little larger than a US quarter. It usually cannot be felt through the skin. A swollen lobe might look or feel like a lump in the front of the neck. A swollen thyroid is called a goiter. Most goiters are caused by not enough iodine in the diet. Iodine is a substance found in shellfish and iodized salt.
Who is at risk?
No one knows the exact causes of thyroid cancer. Doctors can seldom explain why one person gets this disease and another does not. However, it is clear that thyroid cancer is not contagious. No one can "catch" cancer from another person.
Research has shown that people with certain risk factors are more likely than others to develop thyroid cancer. A risk factor is anything that increases a person's chance of developing a disease.
The following risk factors are associated with an increased chance of developing thyroid cancer:
One important source of radiation exposure is treatment with X-rays. Between the 1920s and the 1950s, doctors used high-dose X-rays to treat children who had enlarged tonsils, acne, and other problems affecting the head and neck. Later, scientists found that some people who had received this kind of treatment developed thyroid cancer. (Routine diagnostic X-rays – such as dental X-rays or chest X-rays – use very small doses of radiation. Their benefits nearly always outweigh their risks. However, repeated exposure could be harmful, so it is a good idea for people to talk with their dentist and doctor about the need for each X-ray and to ask about the use of shields to protect other parts of the body.)
Another source of radiation is radioactive fallout. This includes fallout from atomic weapons testing (such as the testing in the United States and elsewhere in the world, mainly in the 1950s and 1960s), nuclear power plant accidents (such as the Chernobyl accident in 1986), and releases from atomic weapons production plants (such as the Hanford facility in Washington state in the late 1940s). Such radioactive fallout contains radioactive iodine (I-131). People who were exposed to one or more sources of I-131, especially if they were children at the time of their exposure, may have an increased risk for thyroid diseases.
A small number of people with a family history of goiter or certain precancerous polyps in the colon are at risk for developing papillary thyroid cancer.
Most people who have known risk factors do not get thyroid cancer. On the other hand, many who do get the disease have none of these risk factors. People who think they may be at risk for thyroid cancer should discuss this concern with their doctor. The doctor may suggest ways to reduce the risk and can plan an appropriate schedule for checkups.
Symptoms
Early thyroid cancer often does not cause symptoms. But as the cancer grows, symptoms may include:
These symptoms are not sure signs of thyroid cancer. An infection, a benign goiter, or another problem also could cause these symptoms. Anyone with these symptoms should see a doctor as soon as possible. Only a doctor can diagnose and treat the problem.
Diagnosis
If a person has symptoms that suggest thyroid cancer, the doctor may perform a physical exam and ask about the patient's personal and family medical history. The doctor also may order laboratory tests and imaging tests to produce pictures of the thyroid and other areas.
The exams and tests may include the following:
If medullary thyroid cancer is suspected, the doctor may check for abnormally high levels of calcium in the blood. The doctor also may order blood tests to detect an altered RET gene or to look for a high level of calcitonin.
The doctor may remove tissue through a needle or during surgery:
- Fine-needle aspiration. For most patients, the doctor removes a sample of tissue from a thyroid nodule with a thin needle. A pathologist looks at the cells under a microscope to check for cancer. Sometimes, the doctor uses an ultrasound device to guide the needle through the nodule.
- Surgical biopsy. If a diagnosis cannot be made from the fine-needle aspiration, the doctor may operate to remove the nodule. A pathologist then checks the tissue for cancer cells.
A person who needs a biopsy may want to ask the doctor the following questions:
Staging the disease
If the diagnosis is thyroid cancer, the doctor needs to know the stage, or extent, of the disease to plan the best treatment. Staging is a careful attempt to learn whether the cancer has spread and, if so, to what parts of the body.
The doctor may use ultrasonography, magnetic resonance imaging (MRI), or computed tomography (CT) to find out whether the cancer has spread to the lymph nodes or other areas within the neck. The doctor may use a nuclear medicine scan of the entire body, such as a radionuclide scan known as the "diagnostic I-131 whole body scan," or other imaging tests to learn whether thyroid cancer has spread to distant sites.

