excessive blood clotting
Lower leg, posterior superficial view.
Excessive blood clotting is a condition in which blood clotting occurs too easily or blood clots don't dissolve properly. Other names for this condition include thrombophilia (mostly used for genetic conditions), hypercoagulability, hypercoagulable disorders or states, thrombotic disorders, and thromboembolic states.
Normally, blood clots form to seal small cuts or breaks on blood vessel walls and stop bleeding. Blood clots also can form due to slow blood flow in the blood vessels. For example, if a blood vessel narrows, blood flow may slow down as it moves through the vessel.
There are many causes of excessive blood clotting. The condition may be due to problems with the blood, blood vessel defects, or other factors. Regardless of the cause, problem blood clots can limit or block blood flow. This can damage the body's organs or even cause death.
Overview
Excessive blood clotting can be acquired or genetic. Acquired causes of
excessive blood clotting are more common than genetic causes.
"Acquired" means that another disease, condition, or factor triggers the
condition. For example, atherosclerosis can damage the blood vessels, which can cause blood clots to form. Other
examples of acquired causes include smoking, overweight
and obesity, and hospitalization.
"Genetic" means the condition is due to an abnormal gene. Most genetic defects that cause excessive blood clotting occur in the proteins needed for blood clotting. Defects also can occur with the substances that delay or dissolve blood clots.
Although the acquired and genetic causes of the condition aren't related, a person can have both. People who are at highest risk for excessive blood clotting have both causes.
Outlook
The outlook and treatment for excessive blood clotting depend on the cause of the blood clots, how severe they are, and how well they can be controlled.
Life-threatening blood clots are treated as emergencies. Medicines that thin the blood are used as routine treatment for blood clotting problems. Some people must take these medicines for the rest of their lives.
With medicines and ongoing care, most people who have excessive blood clotting can successfully manage it.
Causes
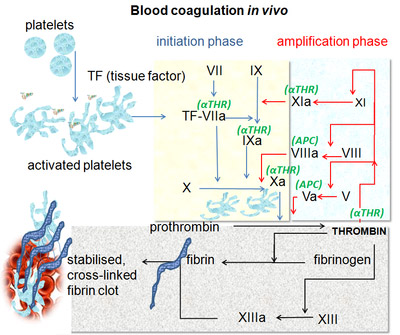
To understand what causes excessive blood clotting, it helps to understand the body's normal blood clotting process.
Normally, blood clots form to seal small cuts or breaks on blood vessel walls and stop bleeding. After the bleeding has stopped and healing has occurred, the body breaks down and removes the clots.
Blood clotting is a complex process, but it mainly involves:
Excessive blood clotting may occur if the body's clotting process is altered or wrongly triggered. Blood clots can form in or travel to the arteries or veins in the brain, heart, kidneys, lungs, and limbs.
Certain diseases and conditions, genetic mutations, medicines, or other factors can cause excessive blood clotting.
Diseases and conditions
A number of diseases and conditions can cause the blood to clot too much or prevent blood clots from dissolving properly. Certain diseases and conditions are more likely to cause clots to form in certain areas of the body.
Antiphospholipid antibody syndrome
Antiphospholipid antibody syndrome, also called APS, is an autoimmune disorder. If you have APS, your body makes antibodies (proteins) that attack phospholipids – a type of fat. Phospholipids are found in all living cells and cell membranes, including blood cells and the lining of blood vessels.
In APS, the antibodies trigger blood clots to form in the body's arteries and veins – the vessels that carry blood to the heart and body. These blood clots can lead to a number of health problems, including frequent miscarriages.
APS is more common in women and people who have other autoimmune or rheumatic disorders, such as lupus.
Bone marrow disorders
Some bone marrow disorders can cause your body to make too many blood cells that can lead to blood clots. Examples of such disorders include polycythemia vera, or PV, and thrombocythemia.
PV is a rare blood disease in which your body makes too many red blood cells. These extra red blood cells make your blood thicker than normal. This slows the flow of blood through your small blood vessels and can lead to blood clots.
Thrombocythemia is a condition in which your body makes too many platelets. The platelets can stick together to form blood clots.
Thrombotic thrombocytopenic purpura and disseminated intravascular coagulation
Two rare, but serious conditions that can cause blood clots are thrombotic thrombocytopenic purpura, or TTP, and disseminated intravascular clotting, or DIC.
TTP causes blood clots to form in the body's small blood vessels, including vessels in the brains, kidneys, and heart.
DIC is a rare complication of pregnancy, severe infections, or severe trauma. DIC causes tiny blood clots to form suddenly throughout the body.
Problems with blood clot breakdown
After a blood clot has done its job, the body normally breaks down the fibrin that holds the clot together.
Several rare genetic and acquired conditions affect the fibrin network that holds blood clots together. Thus, the clots don't break down properly and they remain in the body longer than needed.
In one condition, for example, the body's fibrin is abnormal and resists being broken down. In another condition, the body has a decreased amount of plasmin. This protein is needed to break down fibrin.
Excessive blood clotting that mainly affects the heart and brain
Any condition that damages the smooth inner surface of the blood vessels
can trigger blood clotting. Many of these conditions are acquired. However,
some genetic problems also can damage the blood vessel walls.
Certain diseases, conditions, or factors may trigger excessive blood clotting
mainly in the arteries and veins of the heart and brain.
Atherosclerosis – a disease in which a fatty material called plaque builds up on the insides of your arteries. Over time, the plaque may crack. Platelets clump together to form blood clots where the cracks are. Atherosclerosis is a major case of damage to the blood vessel walls.
Vasculitis – a disorder that causes the body's blood vessels to become inflamed. Platelets may stick where the arteries are damaged, and blood clots can form. Vasculitis also is a major cause of damage to the blood vessel walls.
Diabetes – increases the risk for plaque buildup in the arteries. Nearly 80 percent of people who have diabetes die from dangerous blood clots. (Seventy-five percent of these deaths are due to complications with the heart and blood vessels.)
Heart failure – a condition in which the heart is damaged or weakened and can't pump enough blood to meet the body's needs. This condition slows blood flow, which can cause blood clots to form.
Atrial fibrillation (AF) – the most common type of arrhythmia. An arrhythmia is a problem with the rate or rhythm of the heartbeat. AF can cause blood to pool in the upper chambers of the heart. This can cause blood clots to form.
Overweight and obesity – refer to a person's overall body weight and where the extra weight comes from. Overweight is having extra body weight from muscle, bone, fat, and/or water. Obesity is having a high amount of extra body fat. These conditions can lead to atherosclerosis, which increases the risk of blood clots.
Excessive blood clotting that mainly affects the limbs
Blood clots can form in the veins deep in the limbs. This condition is called deep vein thrombosis (DVT). It mostly affects the deep veins of the legs.
A blood clot in a deep vein can break off and travel through the bloodstream. When the clot travels to the lungs and blocks blood flow, the condition is called pulmonary embolism, or PE.
Certain diseases, conditions, or factors may trigger excessive blood clotting mainly in the deep veins of the limbs. These include:
Genetic mutations
Genetic causes of excessive blood clotting are most often due to gene mutations (changes to a normal gene).
Common mutations include Factor V Leiden and Prothrombin G20210A mutations. Fairly rare genetic mutations include proteins C and S deficiencies and antithrombin III deficiency.
Medicines
Some medicines can disrupt the body's normal blood clotting process. Medicines containing the female hormone estrogen are linked to an increased risk of blood clots. Examples of medicines that may contain estrogen include birth control pills and hormone replacement therapy.
Heparin is a medicine commonly used to prevent blood clots. But, in some people, the medicine can cause blood clots and a low platelet count. This condition is called heparin-induced thrombocytopenia (HIT).
HIT rarely occurs outside of a hospital, because heparin usually is given in hospitals. In HIT, the body's immune system attacks the heparin and a protein on the surface of the platelets. This attack prompts the platelets to start forming blood clots.
Other factors that can alter the blood clotting process
A number of other factors also can alter the clotting process and lead to excessive blood clotting. Common examples include:
Who is at risk?
People at highest risk for excessive blood clotting have both acquired and genetic risk factors. For example, if you have the Factor V Leiden mutation and atherosclerosis, and you smoke, you're at higher risk than someone who has only one of these risk factors.
Genetic risk factors
You're more likely to have a genetic cause of excessive blood clotting if you have:
Factor V Leiden is one of the more common genetic mutations that can alter the blood clotting process. It's found in 5 to 15 percent of the general population. This mutation accounts for up to a quarter of the cases of genetic blood clotting disorders. Factor V Leiden is found mostly in people who have a European background.
Other risk factors
Another risk factor for excessive blood clotting is antiphospholipid antibody syndrome linked to lupus. This condition may affect 4 to 14 percent of the U.S. population.
Signs and symptoms
Signs and symptoms of excessive blood clotting depend on where the clots form. For example, symptoms of a blood clot in the heart or lungs may include chest pain, shortness of breath, and upper body discomfort in the arms, back, neck, or jaw. These symptoms may suggest heart attack or pulmonary embolism (PE).
Signs and symptoms of a blood clot in the deep veins of the leg may include pain, redness, warmth, and swelling in the lower leg. These signs and symptoms may suggest deep vein thrombosis (DVT).
Signs and symptoms of a blood clot in the brain may include headaches, speech changes, paralysis (an inability to move), dizziness, and trouble speaking and understanding. These signs and symptoms may suggest a stroke.
If you have any of these signs or symptoms, call your doctor right away. The cause of the blood clot(s) needs to be found and treated as soon as possible. You may need emergency care.
Complications of blood clots
Blood clots can form in or travel to the arteries or veins in the brain, heart, kidneys, lungs, and limbs. Blood clots can limit or block blood flow. This can damage the body's organs and cause a number of problems. In some cases, blood clots can be fatal.
Stroke
A blood clot in the brain can cause a stroke. A stroke occurs when blood flow to your brain is cut off. If blood flow is cut off for more than a few minutes, the cells in your brain start to die. This impairs the parts of the body that the brain cells control.
A stroke can cause lasting brain damage, long-term disability, paralysis (an inability to move), or death.
Heart attack
A blood clot in the heart can lead to a heart attack. A heart attack occurs when blood flow to a section of heart muscle becomes blocked. If the flow of blood isn't restored quickly, the section of heart muscle becomes damaged from lack of oxygen and begins to die.
This heart damage may not be obvious, or it may cause severe or long-lasting
problems such as heart failure or arrhythmias (irregular heartbeats).
Kidney problems and kidney failure
A blood clot in the kidneys can lead to kidney problems or kidney failure. Kidney failure occurs when the kidneys can no longer remove fluids and waste from your body.
This causes a buildup of these fluids and waste in your body, high blood pressure, and other health problems.
Pulmonary embolism
If a blood clot travels from a deep vein in the body to the lungs, it's called a pulmonary embolism, or PE. PE is a serious condition that can damage your lungs and other organs and cause low oxygen levels in your blood.
Deep vein thrombosis
A blood clot in a vein deep in your arm or leg can cause pain, swelling, redness, or increased warmth in the affected limb. This type of clot is called deep vein thrombosis, or DVT. These clots also can break off, travel to the lungs, and cause PE.
Pregnancy-related problems
Blood clots can cause miscarriages, stillbirths, and other pregnancy-related problems, such as preeclampsia. Preeclampsia is high blood pressure that occurs during pregnancy.
Diagnosis
If your doctor thinks that you have excessive blood clotting based on your signs and symptoms, he or she will look for the cause of the condition.
Your doctor will ask about your medical and family histories and review the results from a physical exam and tests.
Your primary care doctor may refer you to a hematologist. This is a doctor who is an expert on blood diseases.
Medical and family histories
Your doctor may ask you detailed questions about your medical history and your family's medical history. He or she may ask whether you or a blood relative:
Physical exam
Your doctor will do a physical exam to see how severe your blood clotting problem is and to look for its possible causes.
Diagnostic tests and procedures
Your doctor may order blood tests to look at your blood cells and the clotting process. If he or she thinks you may have a genetic condition, you may need more blood tests.
Tests to find the cause of excessive blood clotting may be delayed for weeks or even months while you receive treatment for a problem blood clot.
Complete blood count and platelet count
An initial blood test will include a complete blood count and a platelet count. These tests measure the number of red and white blood cells and platelets in your blood.
In this situation, your doctor will want to know the number of platelets in your blood. Platelets are blood cell fragments that stick together to form clots.
Tests for clotting factors and clotting time
You also may need blood tests that look at the proteins active in the blood clotting process and how long it takes them to form a blood clot.
Clotting proteins or factors react with each other along two pathways called the intrinsic and extrinsic pathways. (A pathway is a string of chemical reactions that always occur in a certain order.) The two pathways join in a common pathway to make a fibrin network that holds blood clots together.
Follow-up tests
If your doctor thinks your blood clotting condition is genetic, you may need other blood tests. These may include tests that check:
Treatment
Excessive blood clotting is treated with medicines. Depending on the size and location of the clot(s), you may need emergency treatment and/or routine treatment.
Emergency treatment
Blood clots can be dangerous. They can damage the body and lead to serious problems, such as stroke, heart attack, kidney failure, deep vein thrombosis, or pulmonary embolism. Blood clots also can cause miscarriages, stillbirths, or pregnancy-related problems.
Emergency treatment to prevent these problems often consists of medicines that can quickly break up clots.
These medicines, called thrombolytics or "clot busters," are used to treat large clots that cause severe symptoms. These medicines can cause sudden bleeding. Thus, they're only used in life-threatening situations.
Routine treatment
Blood thinners
Anticoagulants, or "blood thinners," are used as routine treatment for excessive blood clotting. These medicines prevent blood clots from forming. They also keep existing blood clots from getting larger.
Warfarin and heparin are two types of blood thinners. Warfarin is given in pill form. (Coumadin® is a common brand name for warfarin.) Heparin is injected into a vein.
Your doctor may treat you with both heparin and warfarin at the same time. Heparin acts quickly. Warfarin takes 2 to 3 days before it starts to work. Once the warfarin starts to work, the heparin is stopped.
Pregnant women will be treated with heparin, because warfarin can harm the fetus.
Sometimes aspirin is used with warfarin. In other cases, aspirin may be used alone. Aspirin also thins the blood and helps prevent blood clots.
Some people must take blood thinners for the rest of their lives if their risk for forming blood clots remains high.
The most common side effect of blood thinners is bleeding. This happens if the medicine thins your blood too much. This side effect can be life threatening. Bleeding can occur inside your body (internal bleeding) or on its surface.
Know the warning signs of internal bleeding, so you can get help right away. They include:
A lot of bleeding after a fall or injury or easy bruising or bleeding also may mean that your blood is too thin. Call your doctor right away if you have any of these signs.
People who are treated with blood thinners usually need regular blood tests, called PT and PTT tests, to check how well their blood is clotting.
These tests also show whether you're taking the right amount of medicine. Your doctor will check to make sure that you're taking enough medicine to prevent clots, but not so much that it causes bleeding.
Other treatments
Short-term treatments may include treatment with antithrombin factor and protein C. Antithrombin factor may be helpful for people who have known antithrombin deficiencies. This treatment is used in special situations, such as before surgery, when there's a very serious blood clot or repeat blood clots.
Some people who have antithrombin deficiencies may need this treatment because heparin doesn't work for them.
Protein C may be given to people who have protein C deficiencies before they receive warfarin. Protein C is given to protect them from skin necrosis – a serious side effect of warfarin. (Skin necrosis destroys and damages the skin cells.)
Prevention
You can't prevent genetic causes of excessive blood clotting. However, you can take steps to control or avoid some acquired risk factors.
Living with excessive blood clotting
If you have excessive blood clotting, you should:
Signs and symptoms
Knowing the signs and symptoms of problem blood clots is important. You should call your doctor right away if you have any of these signs or symptoms. The cause of the blood clots needs to be found and treated as soon as possible. You may need emergency care.
Medicines
You may need to take anticoagulants, or "blood thinners," to prevent blood clots or to keep them from getting larger. You should take these medicines exactly as your doctor prescribes.
Tell your doctor about all other medicines you're taking, including over-the-counter medicines. Some medicines can thin your blood. Taking two medicines that thin your blood may increase your risk of bleeding.
Sexually active women who take warfarin (a type of blood thinner) should use birth control measures. This is because warfarin can cause birth defects.
If you need surgery, your doctor may adjust the amount of medicines you take before, during, and after the surgery to prevent bleeding. This also may happen for dental work, but it's less common.
If you take blood thinners, let everyone on your health care team know.
Ongoing care
Have blood tests done as your doctor directs. These tests help track how well your blood is clotting.
The medicines used to treat excessive blood clotting may cause bleeding. Bleeding can occur inside your body (internal bleeding) or on its surface. Know the warning signs of internal bleeding, so you can get help right away. They include:
A lot of bleeding after a fall or injury or easy bruising or bleeding also may mean that your blood is too thin. Call your doctor right away if you have any of these signs.
Talk to your doctor about lifestyle changes that can help you stay healthy. Ask him or her whether your diet may interfere with your medicines. If you take warfarin, some foods or drinks can increase or decrease the effect of the medicine.
Discuss with your doctor what amount of alcohol is safe for you to drink if you're taking medicine. If you smoke, ask your doctor about programs and products that can help you quit.


