lower back pain
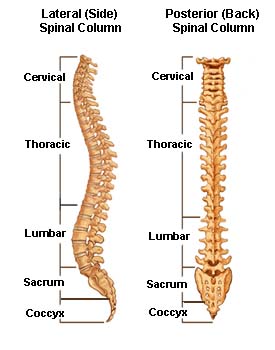
Spinal column.
Back pain is the second most common neurological ailment in the United States – only headache is more common. Fortunately, most occurrences of lower back pain go away within a few days. Others take much longer to resolve or lead to more serious conditions.
Acute or short-term low back pain generally lasts from a few days to a few weeks. Most acute back pain is mechanical in nature – the result of trauma to the lower back or a disorder such as arthritis. Pain from trauma may be caused by a sports injury, work around the house or in the garden, or a sudden jolt such as a car accident or other stress on spinal bones and tissues. Symptoms may range from muscle ache to shooting or stabbing pain, limited flexibility and/or range of motion, or an inability to stand straight. Occasionally, pain felt in one part of the body may "radiate" from a disorder or injury elsewhere in the body. Some acute pain syndromes can become more serious if left untreated.
Chronic back pain is measured by duration – pain that persists for more than 3 months is considered chronic. It is often progressive and the cause can be difficult to determine.
Structures in the back
The back is an intricate structure of bones, muscles, and other tissues that form the posterior part of the body's trunk, from the neck to the pelvis. The centerpiece is the spinal column, which not only supports the upper body's weight but houses and protects the spinal cord – the delicate nervous system structure that carries signals that control the body's movements and convey its sensations. Stacked on top of one another are more than 30 bones – the vertebrae – that form the spinal column, also known as the spine. Each of these bones contains a roundish hole that, when stacked in register with all the others, creates a channel that surrounds the spinal cord. The spinal cord descends from the base of the brain and extends in the adult to just below the rib cage. Small nerves, called nerve roots enter and emerge from the spinal cord through spaces between the vertebrae. Because the bones of the spinal column continue growing long after the spinal cord reaches its full length in early childhood, the nerve roots to the lower back and legs extend many inches down the spinal column before exiting. This large bundle of nerve roots was dubbed by early anatomists as the cauda equina, or horse's tail. The spaces between the vertebrae are maintained by round, spongy pads of cartilage called intervertebral disks that allow for flexibility in the lower back and act much like shock absorbers throughout the spinal column to cushion the bones as the body moves. Bands of tissue known as ligaments and tendons hold the vertebrae in place and attach the muscles to the spinal column.
Starting at the top, the spine has four regions:
The lumbar region of the back, where most back pain is felt, supports the weight of the upper body.
Causes of lower back pain
As people age, bone strength and muscle elasticity and tone tend to decrease. The disks begin to lose fluid and flexibility, which decreases their ability to cushion the vertebrae.
Pain can occur when, for example, someone lifts something too heavy or overstretches, causing a sprain, strain, or spasm in one of the muscles or ligaments in the back. If the spine becomes overly strained or compressed, a disk may rupture or bulge outward. This rupture may put pressure on one of the more than 50 nerves rooted to the spinal cord that control body movements and transmit signals from the body to the brain. When these nerve roots become compressed or irritated, back pain results.
Low back pain may reflect nerve or muscle irritation or bone lesions. Most low back pain follows injury or trauma to the back, but pain may also be caused by degenerative conditions such as arthritis or disk disease, osteoporosis or other bone diseases, viral infections, irritation to joints and disks, or congenital abnormalities in the spine. Obesity, smoking, weight gain during pregnancy, stress, poor physical condition, posture inappropriate for the activity being performed, and poor sleeping position also may contribute to low back pain. Additionally, scar tissue created when the injured back heals itself does not have the strength or flexibility of normal tissue. Buildup of scar tissue from repeated injuries eventually weakens the back and can lead to more serious injury.
Occasionally, low back pain may indicate a more serious medical problem. Pain accompanied by fever or loss of bowel or bladder control, pain when coughing, and progressive weakness in the legs may indicate a pinched nerve or other serious condition. People with diabetes may have severe back pain or pain radiating down the leg related to neuropathy. People with these symptoms should contact a doctor immediately to help prevent permanent damage.
Who is at risk?
Nearly everyone has low back pain sometime. Men and women are equally affected. It occurs most often between ages 30 and 50, due in part to the aging process but also as a result of sedentary life styles with too little (sometimes punctuated by too much) exercise. The risk of experiencing low back pain from disk disease or spinal degeneration increases with age.
Low back pain unrelated to injury or other known cause is unusual in pre-teen children. However, a backpack overloaded with schoolbooks and supplies can quickly strain the back and cause muscle fatigue. The U.S. Consumer Product Safety Commission estimates that more than 13,260 injuries related to backpacks were treated at doctors' offices, clinics, and emergency rooms in the year 2000. To avoid back strain, children carrying backpacks should bend both knees when lifting heavy packs, visit their locker or desk between classes to lighten loads or replace books, or purchase a backpack or airline tote on wheels.
Conditions associated with low back pain
Conditions that may cause low back pain and require treatment by a physician or other health specialist include:
Bulging disk (also called protruding, herniated, or ruptured disk). The intervertebral disks are under constant pressure. As disks degenerate and weaken, cartilage can bulge or be pushed into the space containing the spinal cord or a nerve root, causing pain. Studies have shown that most herniated disks occur in the lower, lumbar portion of the spinal column.
A much more serious complication of a ruptured disk is cauda equina syndrome (see cauda equina, which occurs when disk material is pushed into the spinal canal and compresses the bundle of lumbar and sacral nerve roots. Permanent neurological damage may result if this syndrome is left untreated.
Sciatica is a condition in which a herniated or ruptured disk presses on the sciatic nerve, the large nerve that extends down the spinal column to its exit point in the pelvis and carries nerve fibers to the leg. This compression causes shock-like or burning low back pain combined with pain through the buttocks and down one leg to below the knee, occasionally reaching the foot. In the most extreme cases, when the nerve is pinched between the disk and an adjacent bone, the symptoms involve not pain but numbness and some loss of motor control over the leg due to interruption of nerve signaling. The condition may also be caused by a tumor, cyst, metastatic disease, or degeneration of the sciatic nerve root.
Spinal degeneration from disk wear and tear can lead to a narrowing of the spinal canal. A person with spinal degeneration may experience stiffness in the back upon awakening or may feel pain after walking or standing for a long time.
Spinal stenosis related to congenital narrowing of the bony canal predisposes some people to pain related to disk disease.
Osteoporosis is a metabolic bone disease marked by progressive decrease in bone density and strength. Fracture of brittle, porous bones in the spine and hips results when the body fails to produce new bone and/or absorbs too much existing bone. Women are four times more likely than men to develop osteoporosis. Caucasian women of northern European heritage are at the highest risk of developing the condition.
Skeletal irregularities produce strain on the vertebrae and supporting muscles, tendons, ligaments, and tissues supported by spinal column. These irregularities include scoliosis, a curving of the spine to the side; kyphosis, in which the normal curve of the upper back is severely rounded; lordosis, an abnormally accentuated arch in the lower back; back extension, a bending backward of the spine; and back flexion, in which the spine bends forward.
Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, fatigue, and multiple tender points, particularly in the neck, spine, shoulders, and hips. Additional symptoms may include sleep disturbances, morning stiffness, and anxiety.
Spondylitis refers to chronic back pain and stiffness caused by a severe infection to or inflammation of the spinal joints. Other painful inflammations in the lower back include osteomyelitis (infection in the bones of the spine) and sacroiliitis (inflammation in the sacroiliac joint).
Diagnosis
A thorough medical history and physical exam can usually identify any dangerous conditions or family history that may be associated with the pain. The patient describes the onset, site, and severity of the pain; duration of symptoms and any limitations in movement; and history of previous episodes or any health conditions that might be related to the pain. The physician will examine the back and conduct neurologic tests to determine the cause of pain and appropriate treatment. Blood tests may also be ordered. Imaging tests may be necessary to diagnose tumors or other possible sources of the pain.
A variety of diagnostic methods are available to confirm the cause of low back pain:
X-ray imaging includes conventional and enhanced methods that can help diagnose the cause and site of back pain. A conventional X-ray, often the first imaging technique used, looks for broken bones or an injured vertebra. A technician passes a concentrated beam of low-dose ionized radiation through the back and takes pictures that, within minutes, clearly show the bony structure and any vertebral misalignment or fractures. Tissue masses such as injured muscles and ligaments or painful conditions such as a bulging disk are not visible on conventional X-rays. This fast, noninvasive, painless procedure is usually performed in a doctor's office or at a clinic.
Discography involves the injection of a special contrast dye into a spinal disk thought to be causing low back pain. The dye outlines the damaged areas on X-rays taken following the injection. This procedure is often suggested for patients who are considering lumbar surgery or whose pain has not responded to conventional treatments. Myelograms also enhance the diagnostic imaging of an X-ray. In this procedure, the contrast dye is injected into the spinal canal, allowing spinal cord and nerve compression caused by herniated disks or fractures to be seen on an x-ray.
Computerized tomography (CT) is a quick and painless process used when disk rupture, spinal stenosis, or damage to vertebrae is suspected as a cause of low back pain. X-rays are passed through the body at various angles and are detected by a computerized scanner to produce two-dimensional slices (1 mm each) of internal structures of the back. This diagnostic exam is generally conducted at an imaging center or hospital.
Magnetic resonance imaging (MRI) is used to evaluate the lumbar region for bone degeneration or injury or disease in tissues and nerves, muscles, ligaments, and blood vessels. MRI scanning equipment creates a magnetic field around the body strong enough to temporarily realign water molecules in the tissues. Radio waves are then passed through the body to detect the "relaxation" of the molecules back to a random alignment and trigger a resonance signal at different angles within the body. A computer processes this resonance into either a three-dimensional picture or a two-dimensional slice of the tissue being scanned, and differentiates between bone, soft tissues and fluid-filled spaces by their water content and structural properties. This noninvasive procedure is often used to identify a condition requiring prompt surgical treatment.
Electrodiagnostic procedures include electromyography (EMG), nerve conduction studies, and evoked potential (EP) studies. EMG assesses the electrical activity in a nerve and can detect if muscle weakness results from injury or a problem with the nerves that control the muscles. Very fine needles are inserted in muscles to measure electrical activity transmitted from the brain or spinal cord to a particular area of the body. With nerve conduction studies the doctor uses two sets of electrodes (similar to those used during an electrocardiogram) that are placed on the skin over the muscles. The first set gives the patient a mild shock to stimulate the nerve that runs to a particular muscle. The second set of electrodes is used to make a recording of the nerve's electrical signals, and from this information the doctor can determine if there is nerve damage. EP tests also involve two sets of electrodes – one set to stimulate a sensory nerve and the other set on the scalp to record the speed of nerve signal transmissions to the brain.
Bone scans are used to diagnose and monitor infection, fracture, or disorders in the bone. A small amount of radioactive material is injected into the bloodstream and will collect in the bones, particularly in areas with some abnormality. Scanner-generated images are sent to a computer to identify specific areas of irregular bone metabolism or abnormal blood flow, as well as to measure levels of joint disease.
Thermography involves the use of infrared sensing devices to measure small temperature changes between the two sides of the body or the temperature of a specific organ. Thermography may be used to detect the presence or absence of nerve root compression.
Ultrasound imaging, also called ultrasound scanning or sonography, uses high-frequency sound waves to obtain images inside the body. The sound wave echoes are recorded and displayed as a real-time visual image. Ultrasound imaging can show tears in ligaments, muscles, tendons, and other soft tissue masses in the back.
Treatment
Most low back pain can be treated without surgery. Treatment involves using analgesics, reducing inflammation, restoring proper function and strength to the back, and preventing recurrence of the injury. Most patients with back pain recover without residual functional loss. Patients should contact a doctor if there is not a noticeable reduction in pain and inflammation after 72 hours of self-care.
Although ice and heat (the use of cold and hot compresses) have never been scientifically proven to quickly resolve low back injury, compresses may help reduce pain and inflammation and allow greater mobility for some individuals. As soon as possible following trauma, patients should apply a cold pack or a cold compress (such as a bag of ice or bag of frozen vegetables wrapped in a towel) to the tender spot several times a day for up to 20 minutes. After 2 to 3 days of cold treatment, they should then apply heat (such as a heating lamp or hot pad) for brief periods to relax muscles and increase blood flow. Warm baths may also help relax muscles. Patients should avoid sleeping on a heating pad, which can cause burns and lead to additional tissue damage.
Bed rest – 1–2 days at most. A 1996 Finnish study found that persons who continued their activities without bed rest following onset of low back pain appeared to have better back flexibility than those who rested in bed for a week. Other studies suggest that bed rest alone may make back pain worse and can lead to secondary complications such as depression, decreased muscle tone, and blood clots in the legs. Patients should resume activities as soon as possible. At night or during rest, patients should lie on one side, with a pillow between the knees (some doctors suggest resting on the back and putting a pillow beneath the knees).
Exercise may be the most effective way to speed recovery from low back pain and help strengthen back and abdominal muscles. Maintaining and building muscle strength is particularly important for persons with skeletal irregularities. Doctors and physical therapists can provide a list of gentle exercises that help keep muscles moving and speed the recovery process. A routine of back-healthy activities may include stretching exercises, swimming, walking, and movement therapy to improve coordination and develop proper posture and muscle balance. Yoga is another way to gently stretch muscles and ease pain. Any mild discomfort felt at the start of these exercises should disappear as muscles become stronger. But if pain is more than mild and lasts more than 15 minutes during exercise, patients should stop exercising and contact a doctor.
Medications are often used to treat acute and chronic low back pain. Effective pain relief may involve a combination of prescription drugs and over-the-counter remedies. Patients should always check with a doctor before taking drugs for pain relief. Certain medicines, even those sold over the counter, are unsafe during pregnancy, may conflict with other medications, may cause side effects including drowsiness, or may lead to liver damage.
Spinal manipulation is literally a hands-on approach in which professionally licensed specialists use leverage and a series of exercises to adjust spinal structures and restore back mobility.
When back pain does not respond to more conventional approaches, patients may consider the following options:
Acupuncture involves the insertion of needles the width of a human hair along precise points throughout the body. Practitioners believe this process triggers the release of naturally occurring painkilling molecules called peptides and keeps the body's normal flow of energy unblocked. Clinical studies are measuring the effectiveness of acupuncture in comparison to more conventional procedures in the treatment of acute low back pain.
Biofeedback is used to treat many acute pain problems, most notably back pain and headache. Using a special electronic machine, the patient is trained to become aware of, to follow, and to gain control over certain bodily functions, including muscle tension, heart rate, and skin temperature (by controlling local blood flow patterns). The patient can then learn to effect a change in his or her response to pain, for example, by using relaxation techniques. Biofeedback is often used in combination with other treatment methods, generally without side effects.
Interventional therapy can ease chronic pain by blocking nerve conduction between specific areas of the body and the brain. Approaches range from injections of local anesthetics, steroids, or narcotics into affected soft tissues, joints, or nerve roots to more complex nerve blocks and spinal cord stimulation. When extreme pain is involved, low doses of drugs may be administered by catheter directly into the spinal cord. Chronic use of steroid injections may lead to increased functional impairment.
Traction involves the use of weights to apply constant or intermittent force to gradually pull the skeletal structure into better alignment. Traction is not recommended for treating acute low back symptoms.
Transcutaneous electrical nerve stimulation (TENS) is administered by a battery-powered device that sends mild electric pulses along nerve fibers to block pain signals to the brain. Small electrodes placed on the skin at or near the site of pain generate nerve impulses that block incoming pain signals from the peripheral nerves. TENS may also help stimulate the brain's production of endorphins (chemicals that have pain-relieving properties).
Ultrasound is a noninvasive therapy used to warm the body's internal tissues, which causes muscles to relax. Sound waves pass through the skin and into the injured muscles and other soft tissues.
Minimally invasive outpatient treatments to seal fractures of the vertebrae caused by osteoporosis include vertebroplasty and kyphoplasty. Vertebroplasty uses three-dimensional imaging to help a doctor guide a fine needle into the vertebral body. A glue-like epoxy is injected, which quickly hardens to stabilize and strengthen the bone and provide immediate pain relief. In kyphoplasty, prior to injecting the epoxy, a special balloon is inserted and gently inflated to restore height to the bone and reduce spinal deformity.
In the most serious cases, when the condition does not respond to other therapies, surgery may relieve pain caused by back problems or serious musculoskeletal injuries. Some surgical procedures may be performed in a doctor's office under local anesthesia, while others require hospitalization. It may be months following surgery before the patient is fully healed, and he or she may suffer permanent loss of flexibility. Since invasive back surgery is not always successful, it should be performed only in patients with progressive neurologic disease or damage to the peripheral nerves.
Other surgical procedures to relieve severe chronic pain include rhizotomy, in which the nerve root close to where it enters the spinal cord is cut to block nerve transmission and all senses from the area of the body experiencing pain; cordotomy, where bundles of nerve fibers on one or both sides of the spinal cord are intentionally severed to stop the transmission of pain signals to the brain; and dorsal root entry zone operation, or DREZ, in which spinal neurons transmitting the patient's pain are destroyed surgically.
Prevention
Recurring back pain resulting from improper body mechanics or other nontraumatic causes is often preventable. A combination of exercises that don't jolt or strain the back, maintaining correct posture, and lifting objects properly can help prevent injuries.
Many work-related injuries are caused or aggravated by stressors such as heavy lifting, contact stress (repeated or constant contact between soft body tissue and a hard or sharp object, such as resting a wrist against the edge of a hard desk or repeated tasks using a hammering motion), vibration, repetitive motion, and awkward posture. Applying ergonomic principles – designing furniture and tools to protect the body from injury – at home and in the workplace can greatly reduce the risk of back injury and help maintain a healthy back. More companies and homebuilders are promoting ergonomically designed tools, products, workstations, and living space to reduce the risk of musculoskeletal injury and pain.
The use of wide elastic belts that can be tightened to pull in lumbar and abdominal muscles to prevent low back pain remains controversial. A landmark study of the use of lumbar support or abdominal support belts worn by persons who lift or move merchandise found no evidence that the belts reduce back injury or back pain. The 2-year study, reported by the National Institute for Occupational Safety and Health (NIOSH) in December 2000, found no statistically significant difference in either the incidence of workers' compensation claims for job-related back injuries or the incidence of self-reported pain among workers who reported they wore back belts daily compared to those workers who reported never using back belts or reported using them only once or twice a month.
Although there have been anecdotal case reports of injury reduction among workers using back belts, many companies that have back belt programs also have training and ergonomic awareness programs. The reported injury reduction may be related to a combination of these or other factors.
Quick tips to a healthier back
Following any period of prolonged inactivity, begin a program of regular low-impact exercises. Speed walking, swimming, or stationary bike riding 30 minutes a day can increase muscle strength and flexibility. Yoga can also help stretch and strengthen muscles and improve posture. Ask your physician or orthopedist for a list of low-impact exercises appropriate for your age and designed to strengthen lower back and abdominal muscles.
Research
Scientists are examining the use of different drugs to effectively treat back pain, in particular daily pain that has lasted at least 6 months. Other studies are comparing different health care approaches to the management of acute low back pain (standard care versus chiropractic, acupuncture, or massage therapy). These studies are measuring symptom relief, restoration of function, and patient satisfaction. Other research is comparing standard surgical treatments to the most commonly used standard nonsurgical treatments to measure changes in health-related quality of life among patients suffering from spinal stenosis. NIH-funded research at the Consortial Center for Chiropractic Research encourages the development of high-quality chiropractic projects. The Center also encourages collaboration between basic and clinical scientists and between the conventional and chiropractic medical communities.
Other researchers are studying whether low-dose radiation can decrease scarring around the spinal cord and improve the results of surgery. Still others are exploring why spinal cord injury and other neurological changes lead to an increased sensitivity to pain or a decreased pain threshold (where normally non-painful sensations are perceived as painful, a class of symptoms called neuropathic pain), and how fractures of the spine and their repair affect the spinal canal and intervertebral foramena (openings around the spinal roots).
Also under study for patients with degenerative disk disease is artificial spinal disk replacement surgery. The damaged disk is removed and a metal and plastic disk about the size of a quarter is inserted into the spine. Ideal candidates for disk replacement surgery are persons between the ages of 20 and 60 who have only one degenerating disk, do not have a systemic bone disease such as osteoporosis, have not had previous back surgery, and have failed to respond to other forms of nonsurgical treatment. Compared to other forms of back surgery, recovery from this form of surgery appears to be shorter and the procedure has fewer complications.


